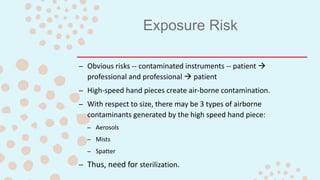
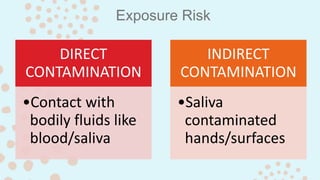
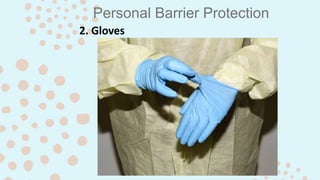
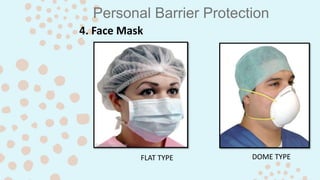
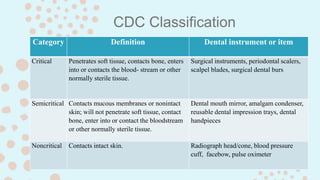
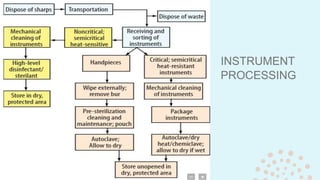
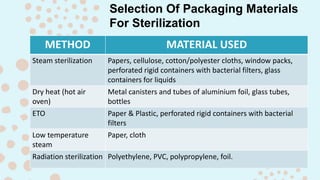
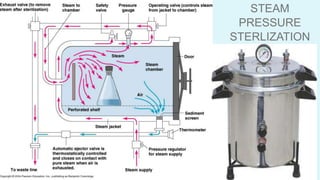
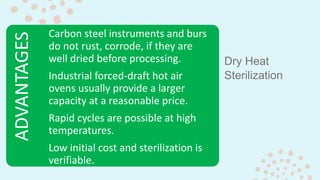
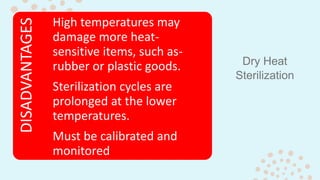
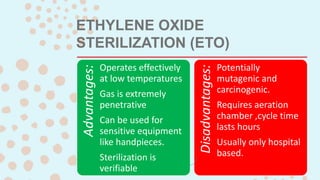
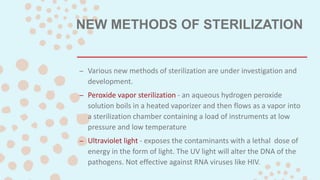
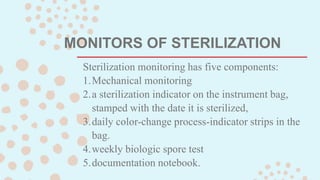
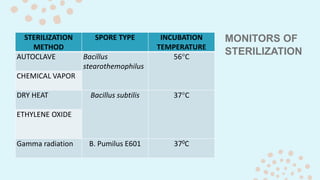
Sterilization and disinfection are important for preventing transmission of diseases between patients and healthcare professionals. Proper cleaning and use of barriers like gloves and masks are required. Instruments must be properly sterilized depending on their risk category using methods like steam, dry heat, or chemicals. Effectiveness is ensured through biological monitoring. Disinfectants and antiseptics are used to clean surfaces and skin but do not guarantee sterilization. Clinical waste requires appropriate disposal to prevent further contamination.