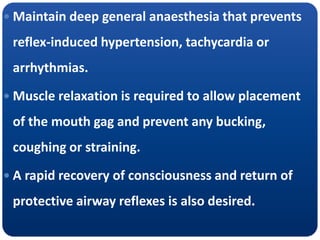
1. Tonsillectomy requires maintaining deep general anesthesia to prevent reflex responses during the procedure while allowing for rapid recovery of airway reflexes.
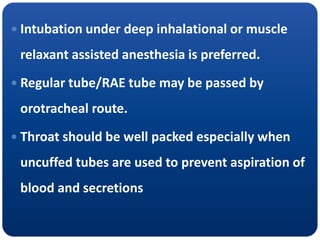
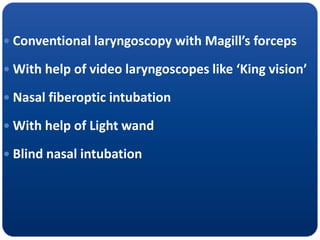
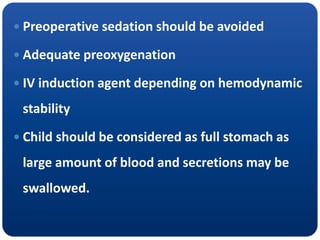
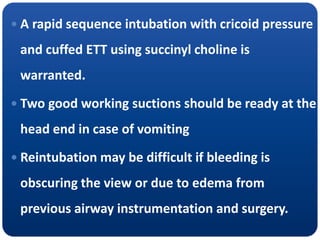
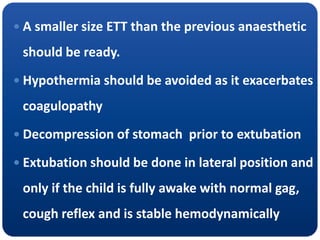
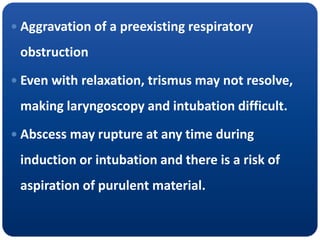
2. Intubation is usually done under deep inhalational or muscle relaxant anesthesia to prevent bucking, and the tube is secured to prevent aspiration of blood or secretions.
3. During the procedure, inhaled anesthetics with opioids or muscle relaxants are used to maintain adequate depth while monitoring for blood loss or airway issues.