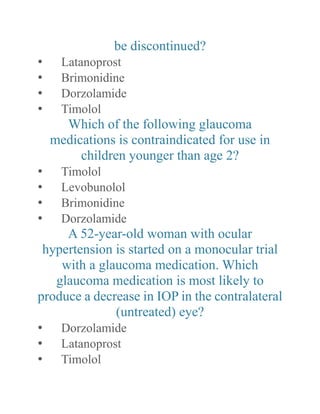
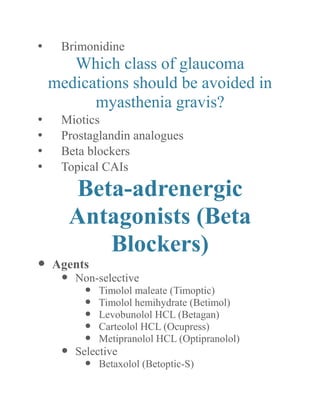
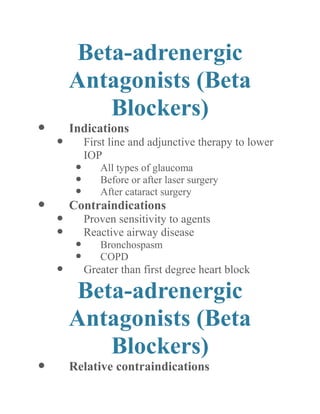
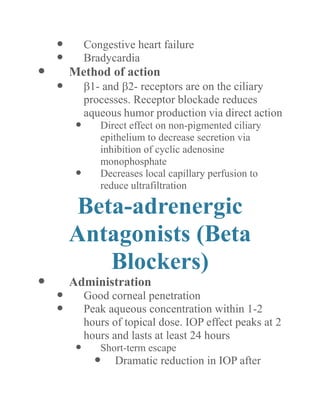
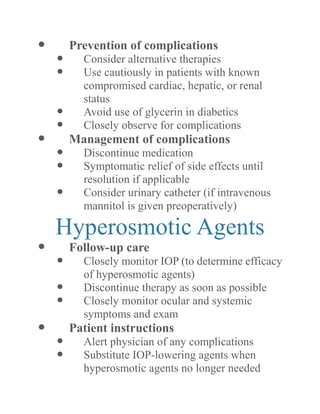
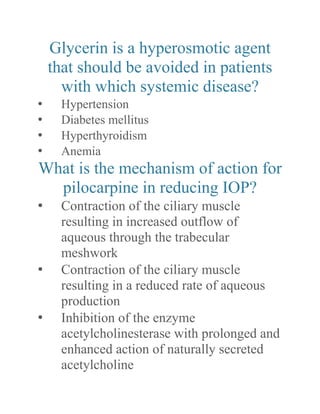
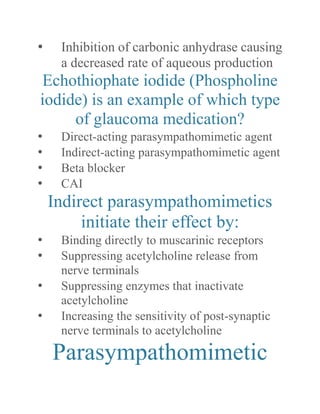
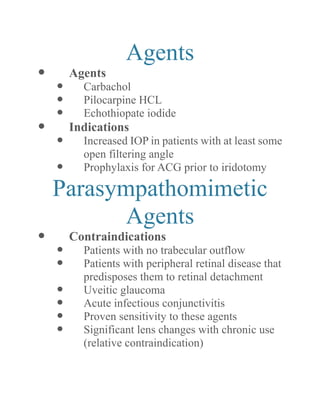
The document discusses various medical treatments for glaucoma, including different drug classes and their mechanisms of action, indications, contraindications and side effects. It provides detailed information on adrenergic agonists, beta-adrenergic antagonists, carbonic anhydrase inhibitors, and combined medications used to treat glaucoma. Key points covered include how the drugs work to lower intraocular pressure, when they should and should not be used, and common adverse effects.