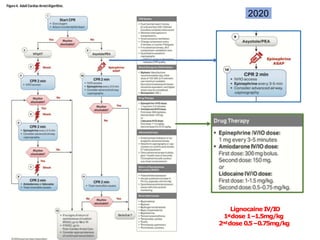
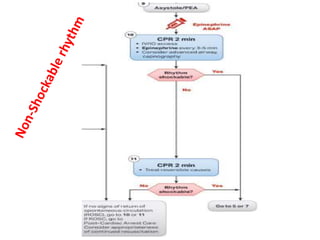
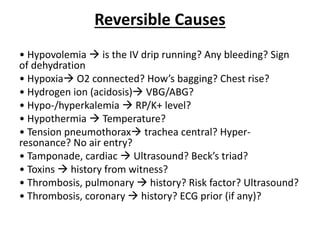
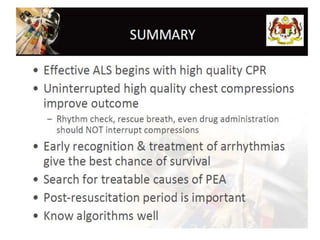
This document summarizes updates to the Advanced Life Support guidelines from 2015 to 2020. Key changes include:
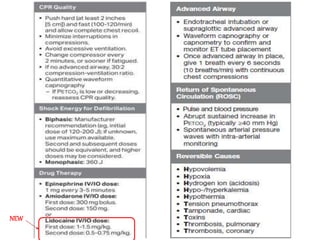
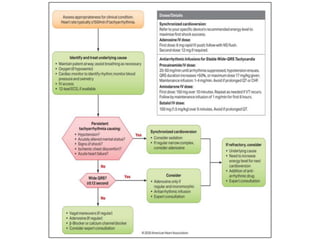
- Lignocaine dosage recommendations for IV/IO administration were updated.
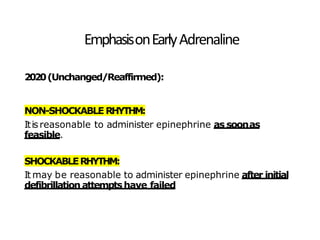
- Emphasis on early adrenaline administration for non-shockable and shockable rhythms.
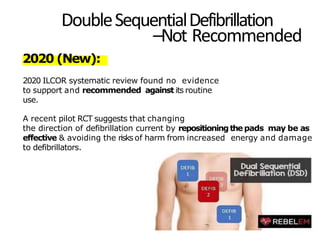
- Double sequential defibrillation is not recommended.
- Standard adrenaline dosing remains 1mg every 3-5 minutes but high dose is not routinely advised.
- Amiodarone and lidocaine can be considered for refractory ventricular fibrillation/pulseless ventricular tachycardia.