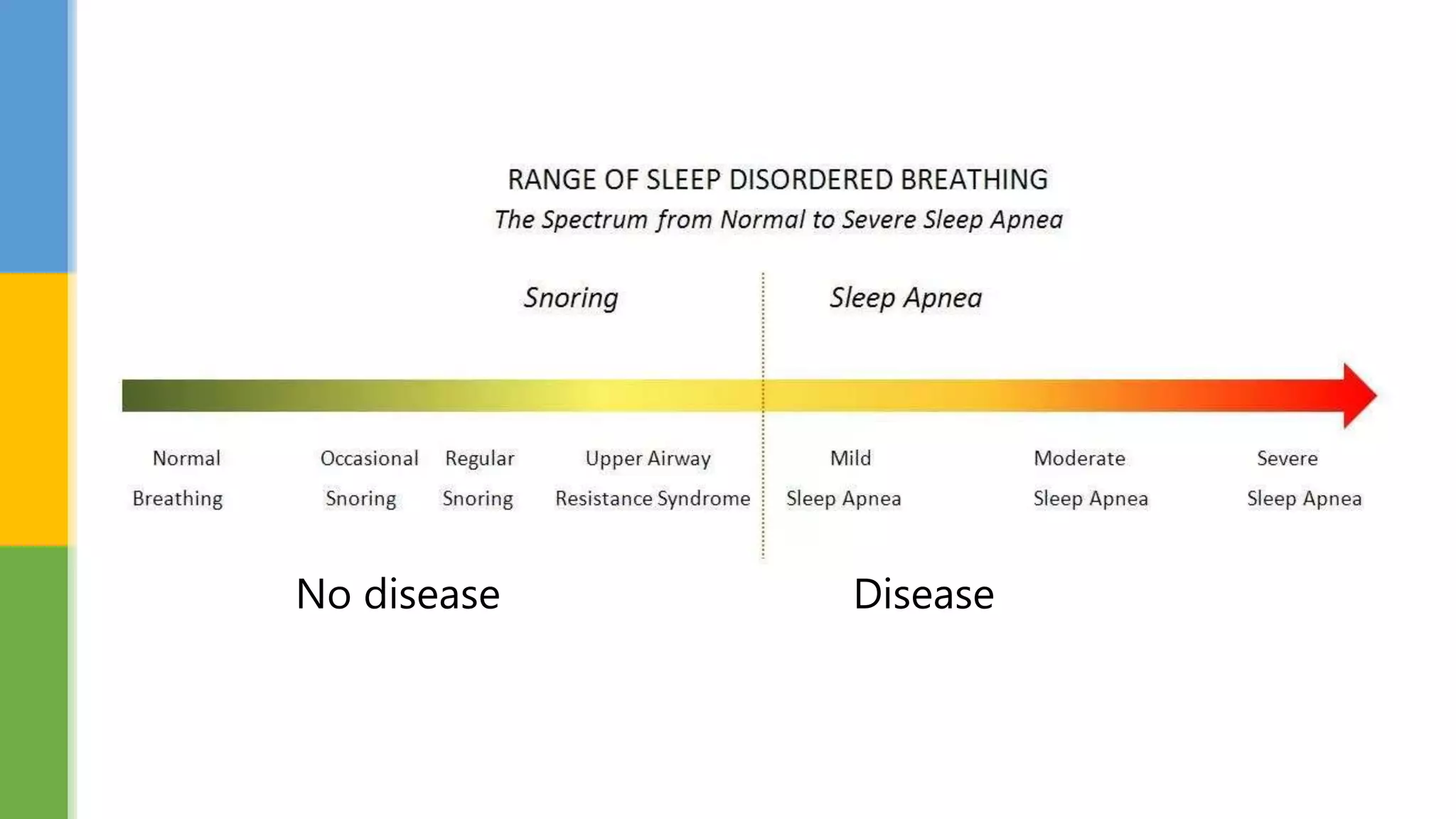
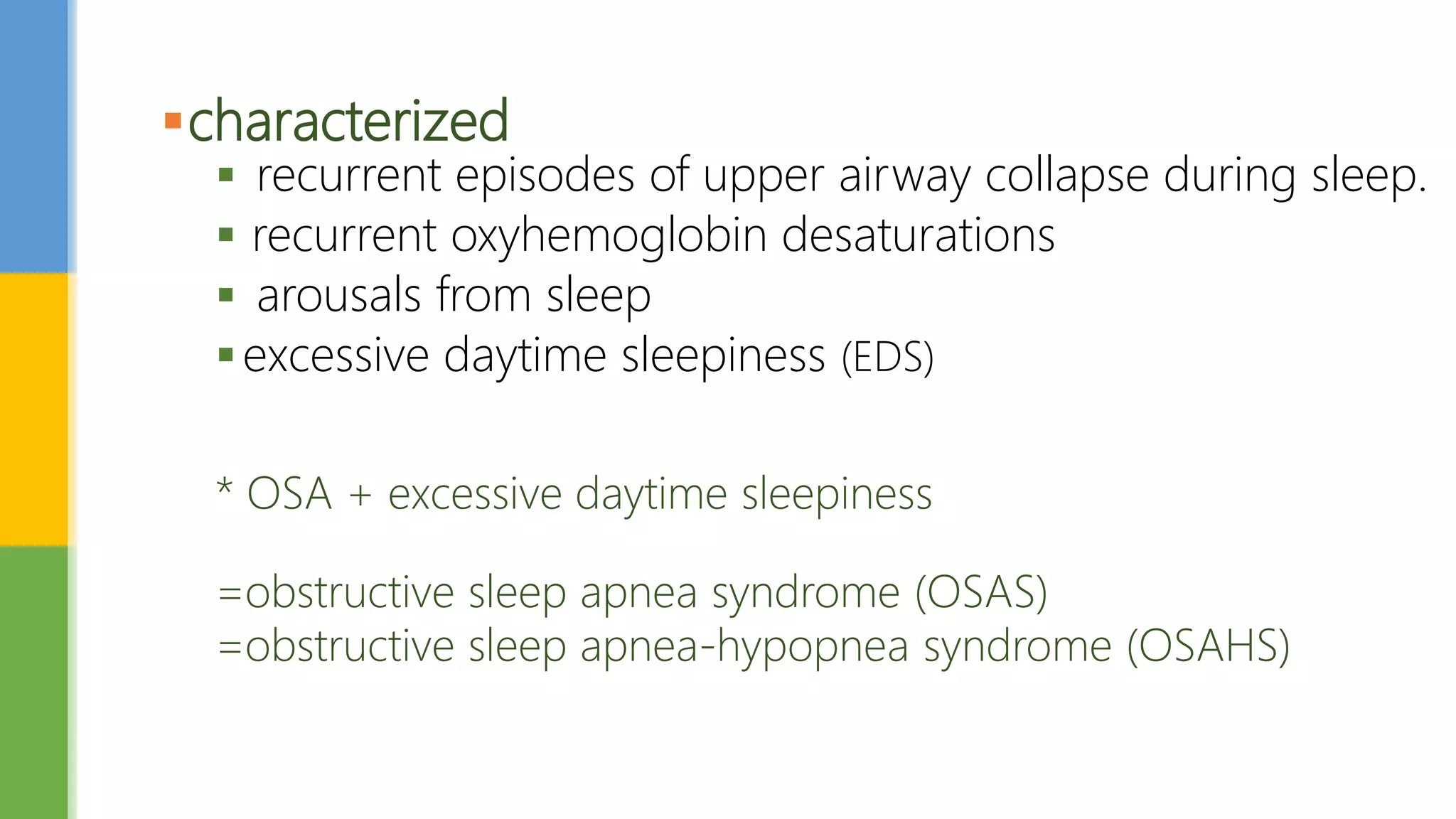
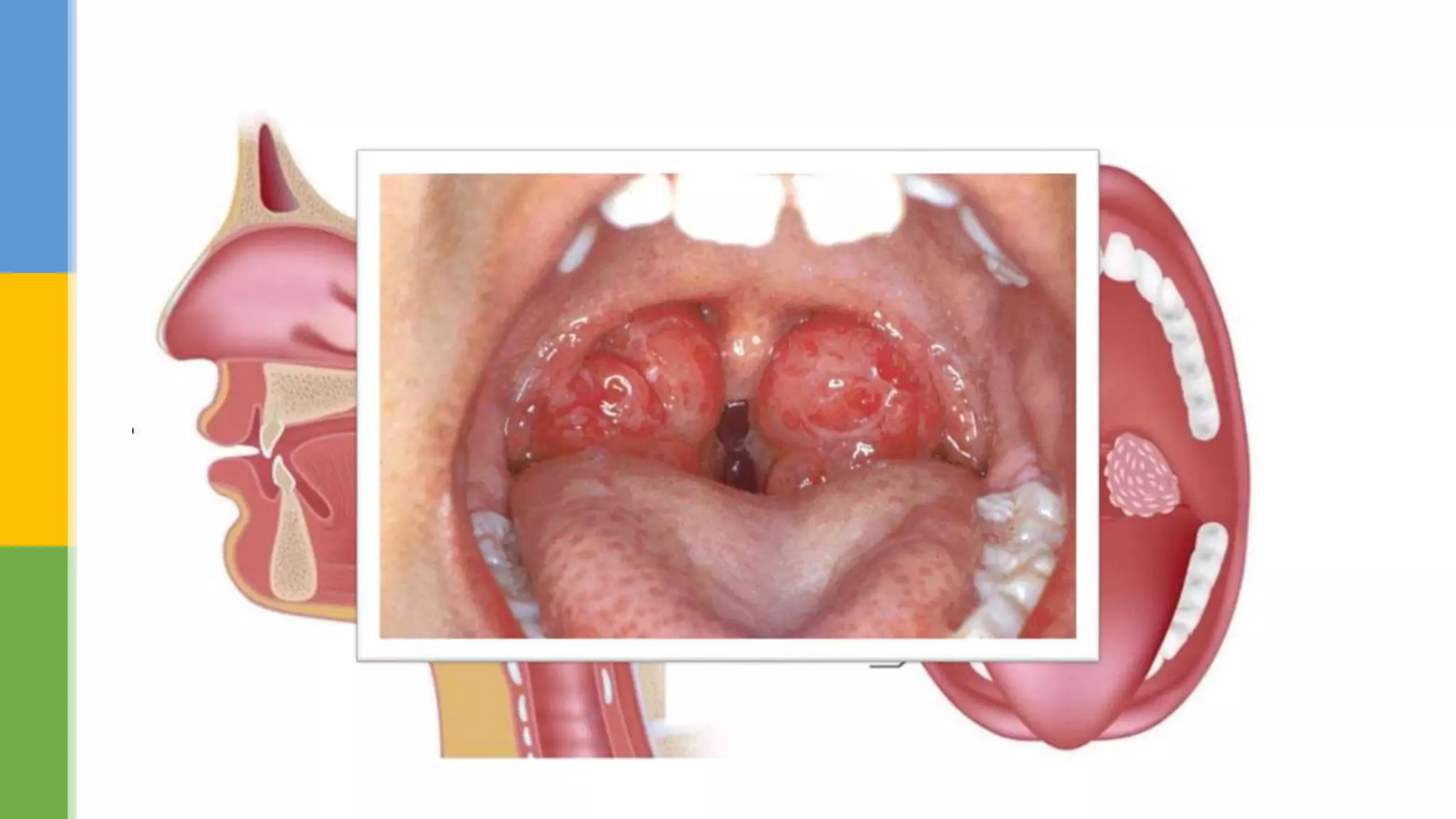
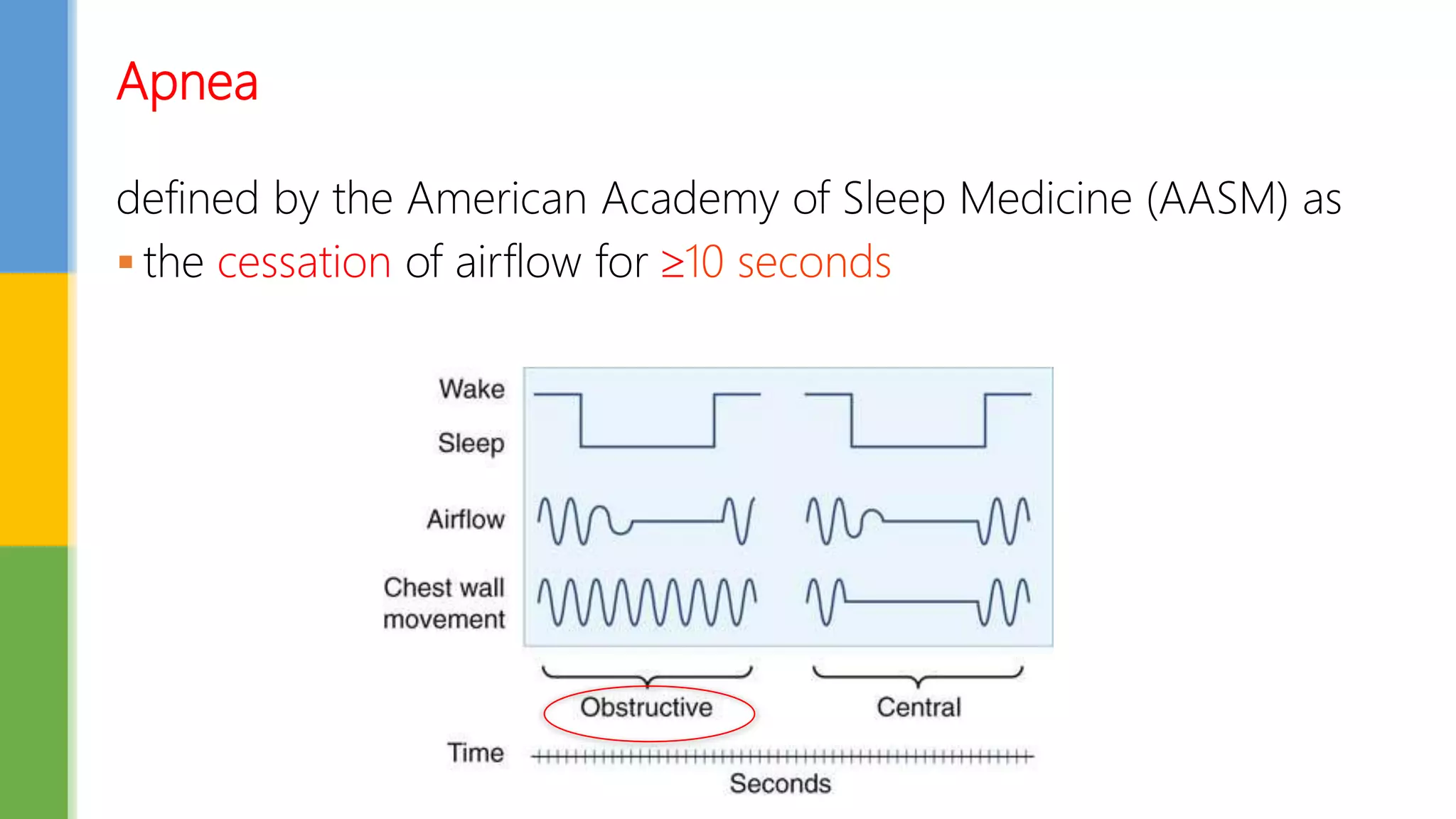
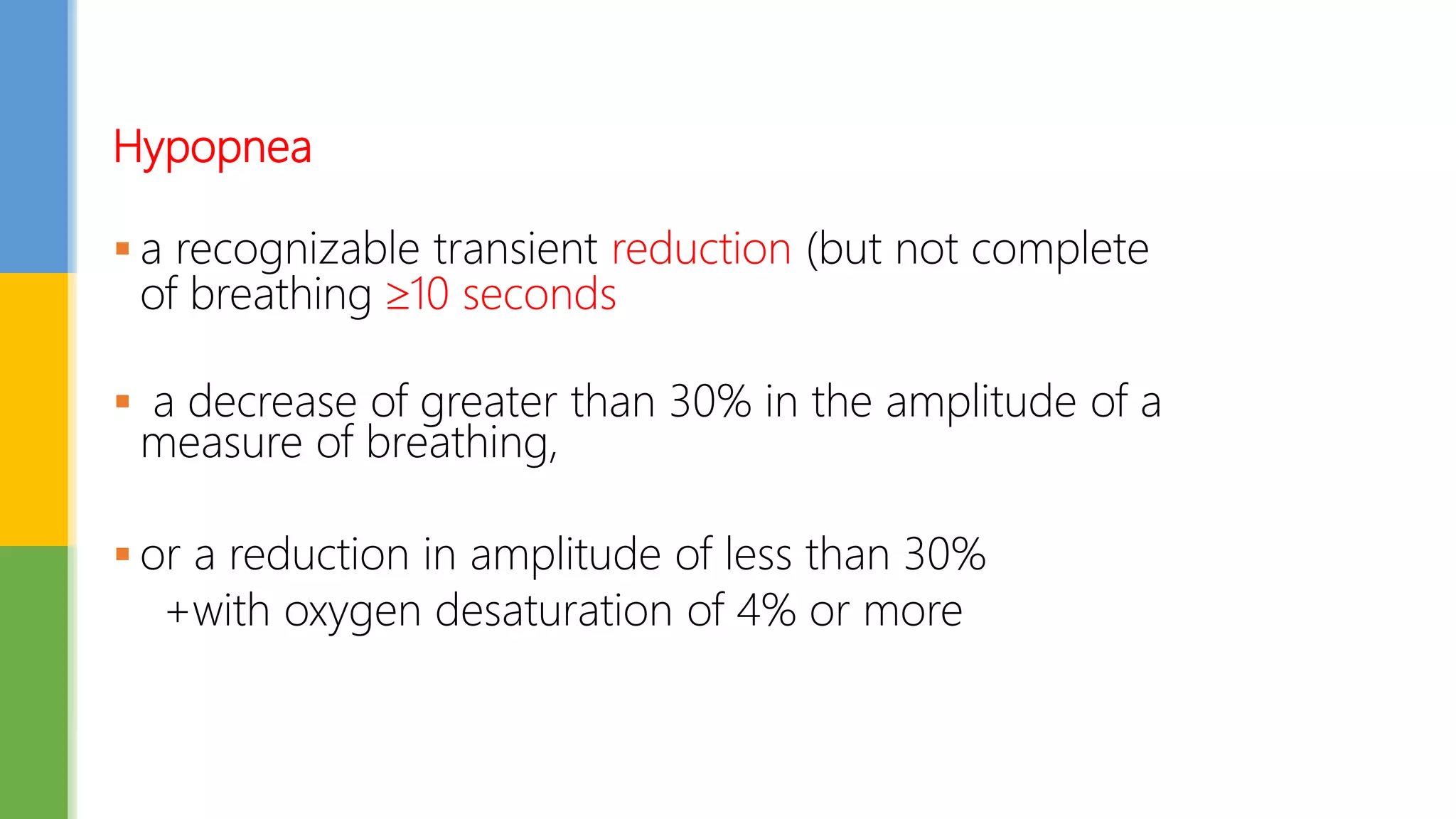
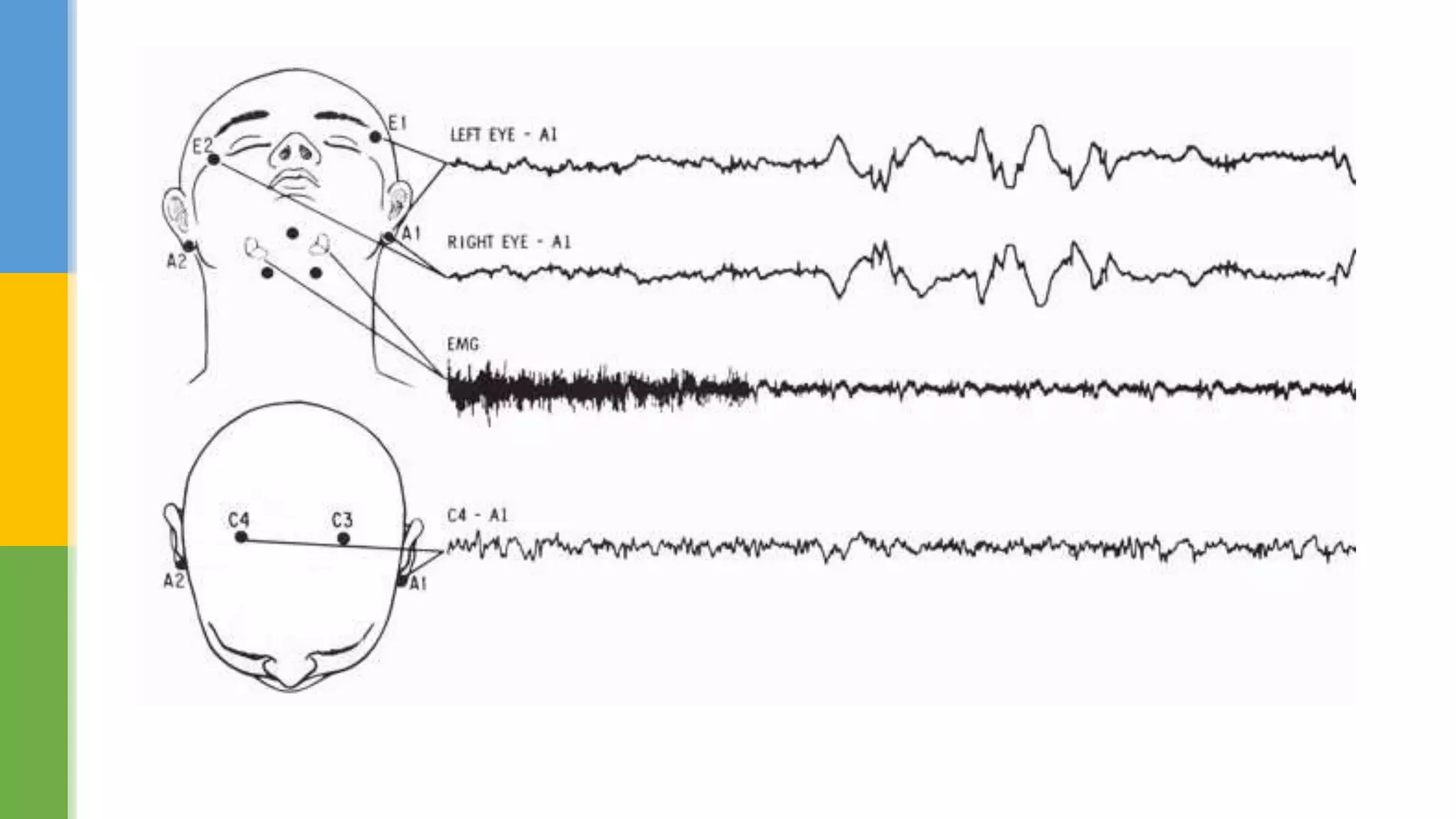
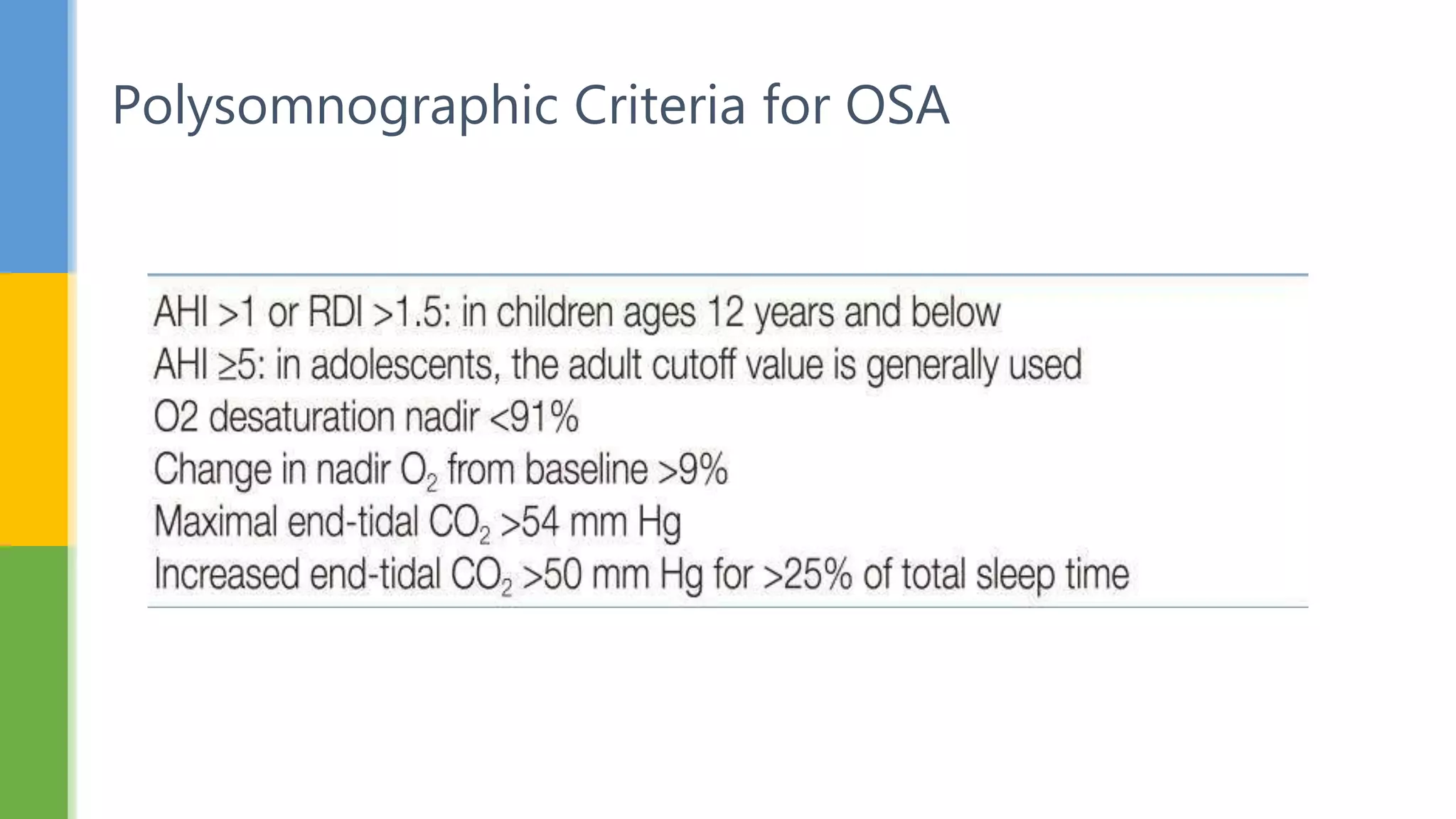
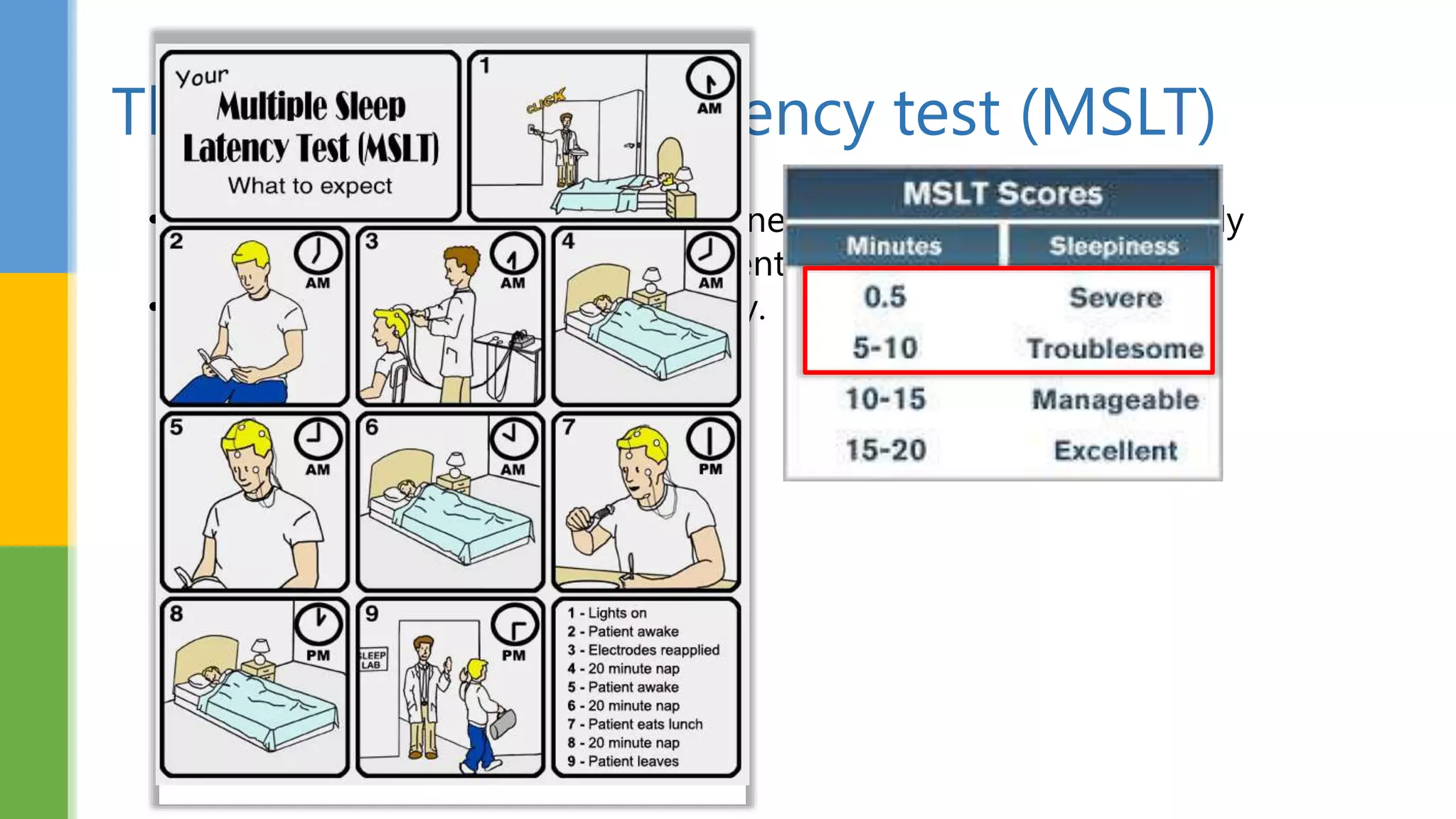
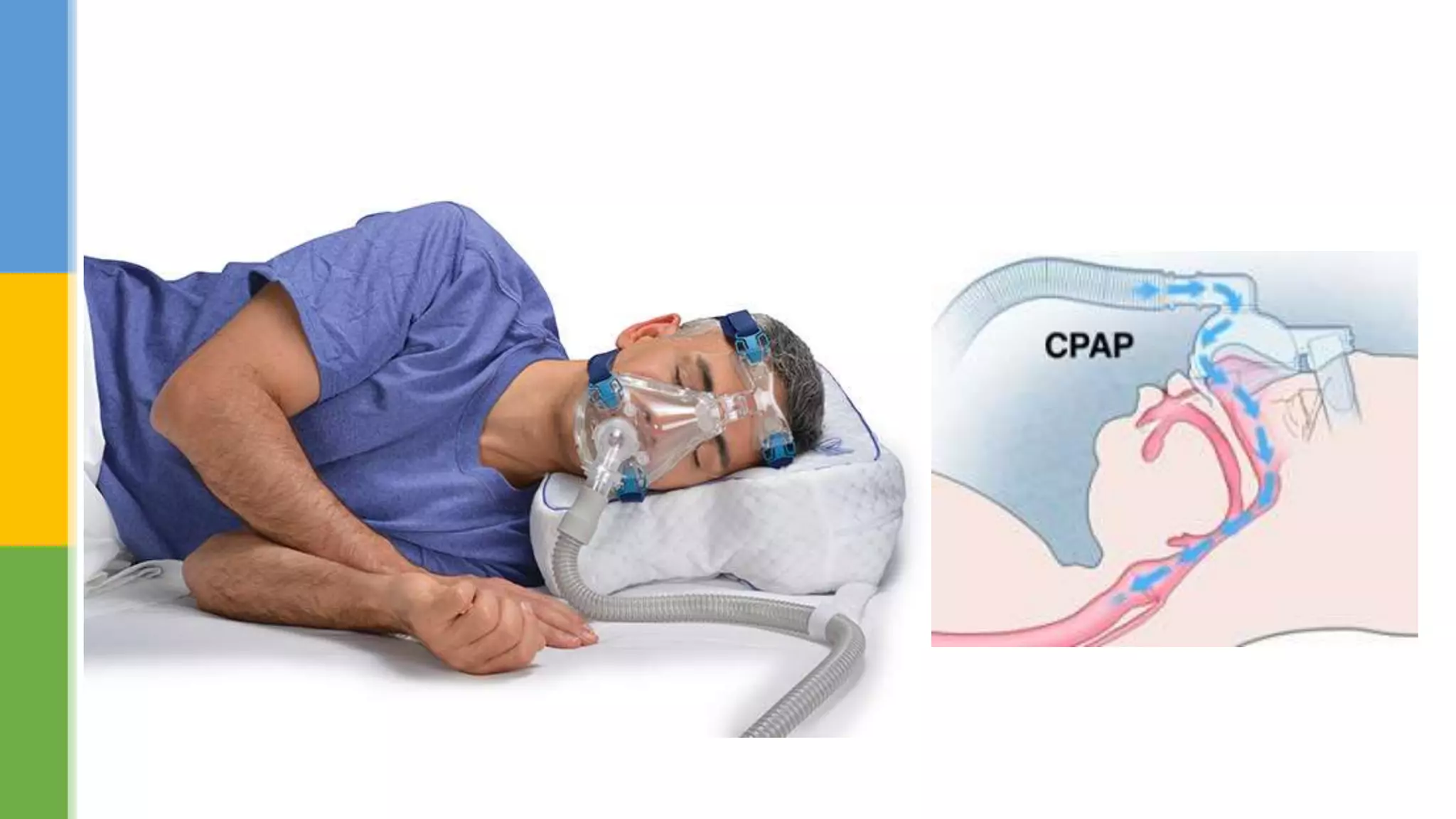
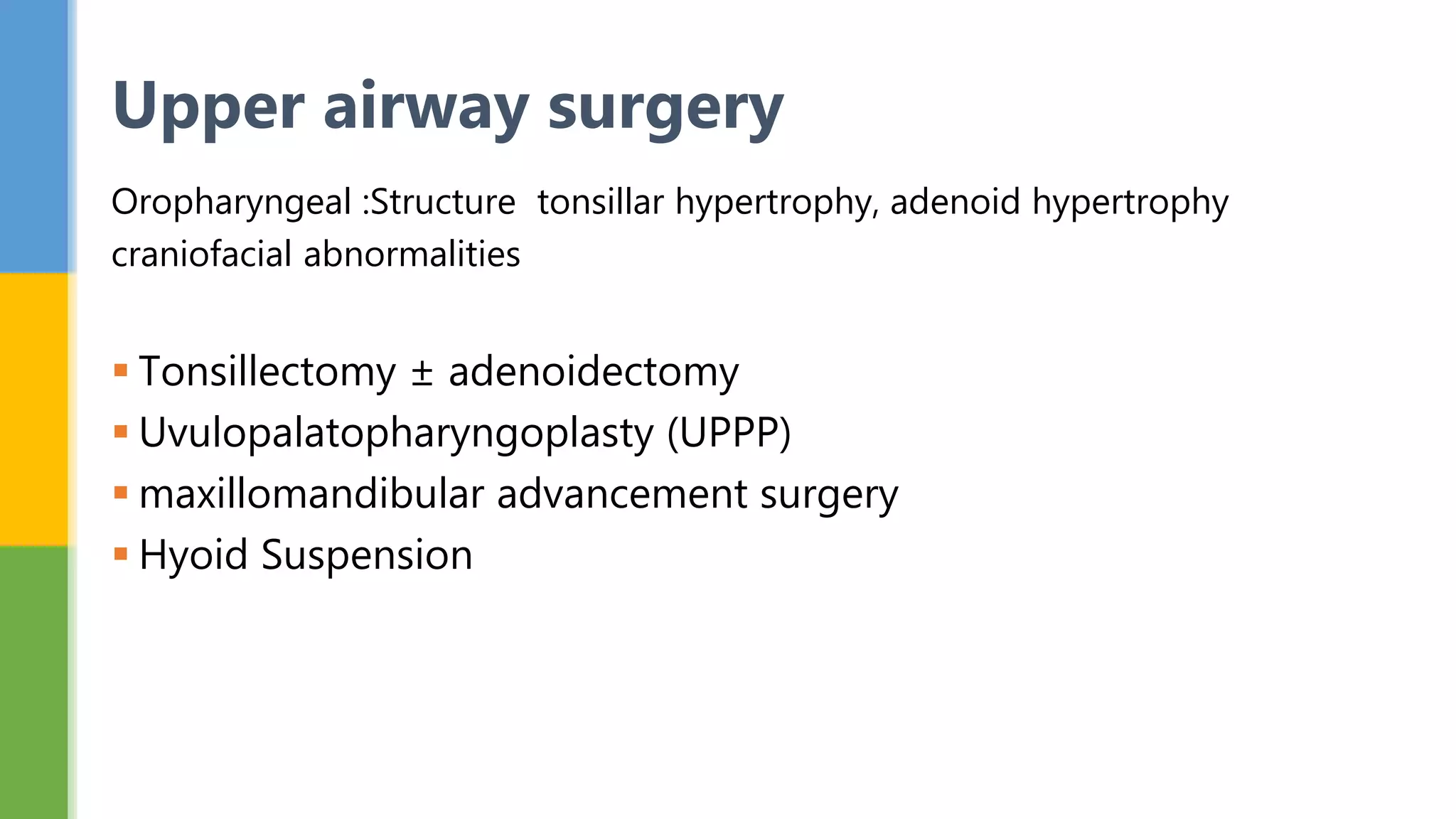
This document provides an overview of obstructive sleep apnea (OSA). It discusses the definition, signs and symptoms, epidemiology, diagnosis using polysomnography, and treatment options including continuous positive airway pressure therapy and upper airway surgery. The key points are that OSA involves recurrent collapse of the upper airway during sleep, leading to pauses in breathing and oxygen level drops. Diagnosis is via an overnight sleep study, and treatment focuses on eliminating airway obstructions through devices, weight loss, or surgery.