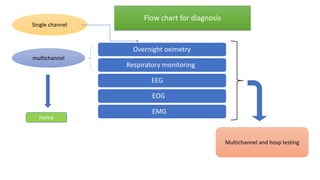
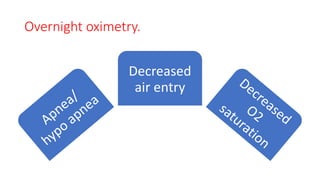
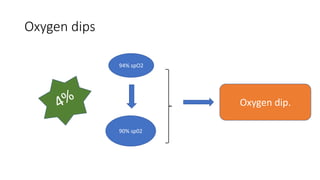
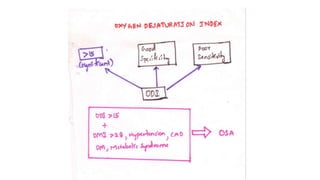
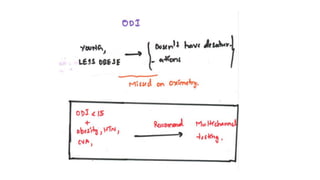
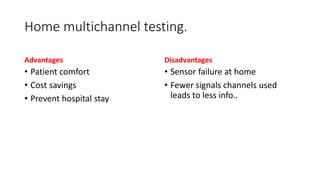
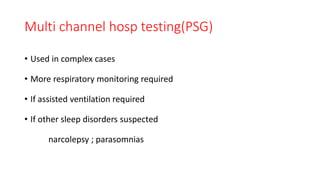
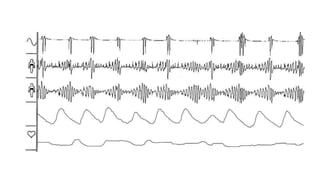
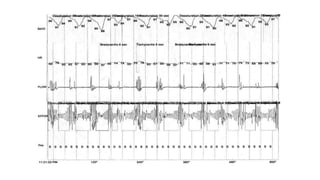
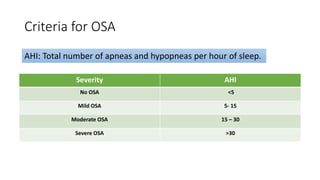
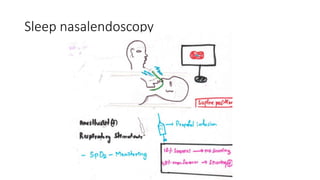
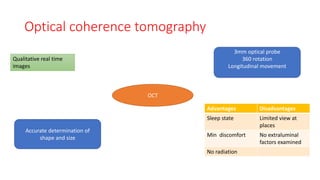
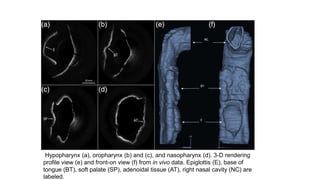
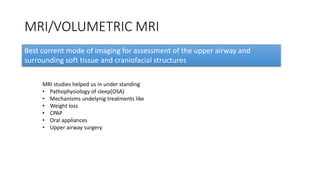
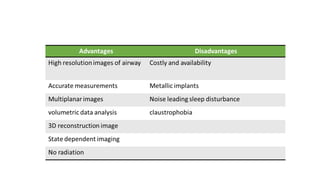
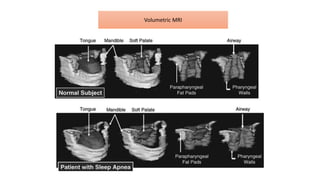
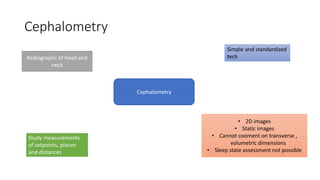
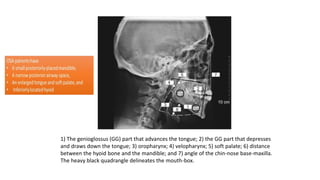
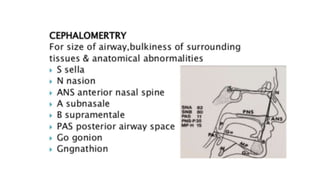
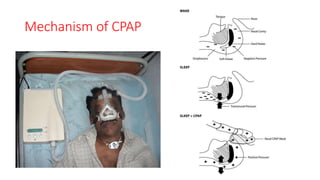
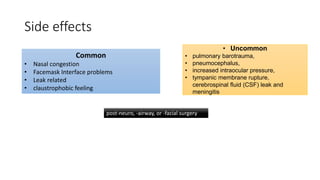
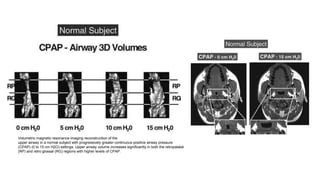
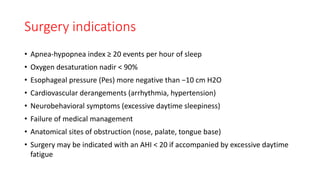
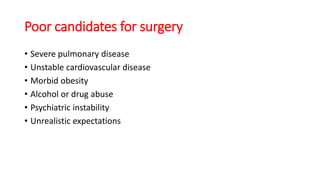
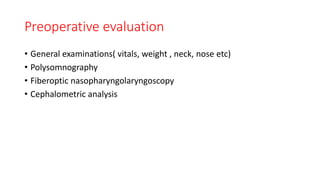
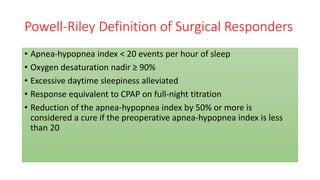
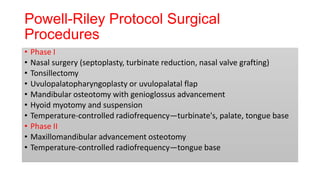
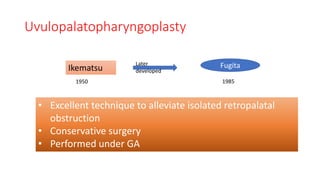
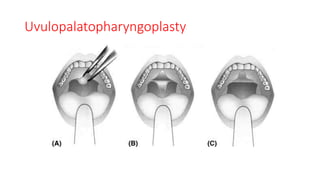
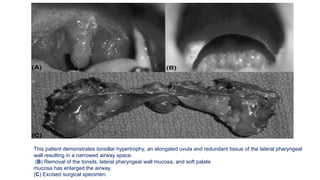
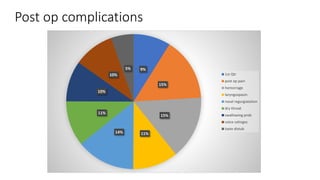
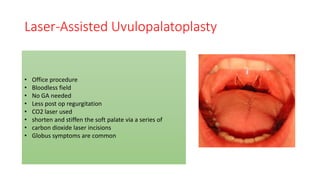
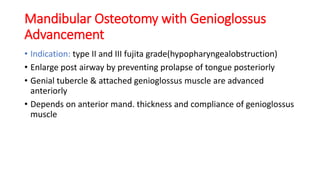
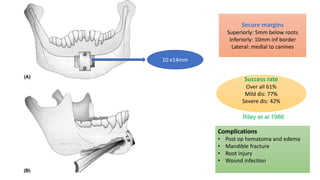
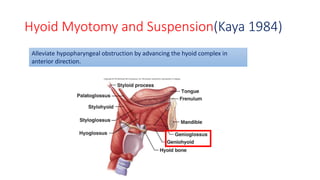
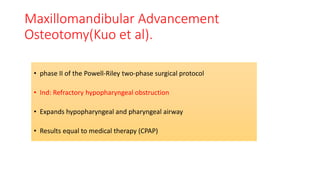
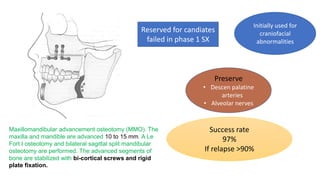
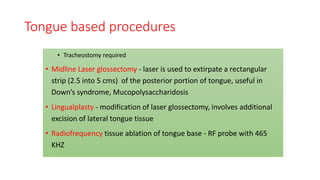
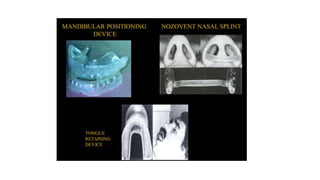
This document discusses the diagnosis and management of obstructive sleep apnea (OSA). It describes various tests used to diagnose OSA including overnight oximetry, polysomnography (PSG), and sleep imaging. It discusses evaluating OSA severity based on the apnea hypopnea index from PSG. Medical management includes continuous positive airway pressure (CPAP) which helps keep the airway open during sleep. Surgical management is considered for severe cases and involves procedures like uvulopalatopharyngoplasty, mandibular advancement, and hyoid surgery to enlarge the airway. Maxillomandibular advancement is reserved for refractory cases. The document provides details on various diagnostic tests, treatments,