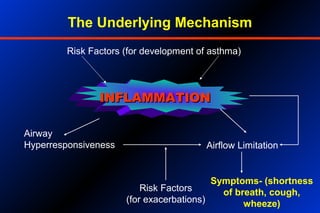
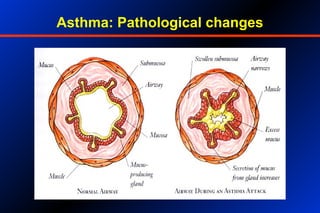
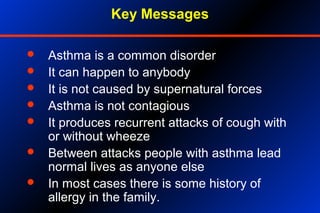
1. Asthma is a chronic inflammatory disorder of the airways that affects 15-20 million people in India. It is characterized by airway hyperresponsiveness and inflammation.
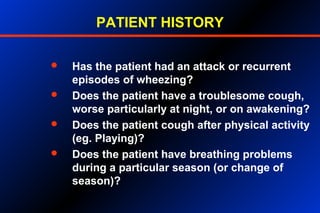
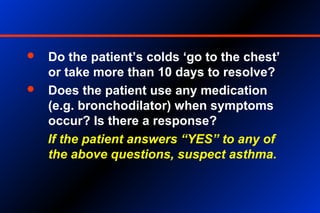
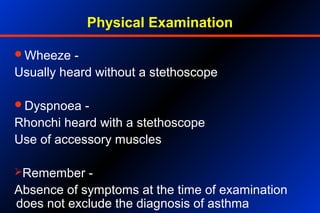
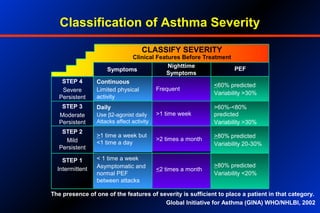
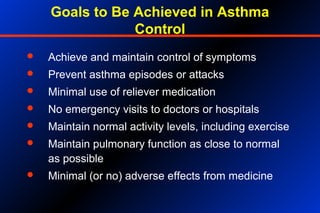
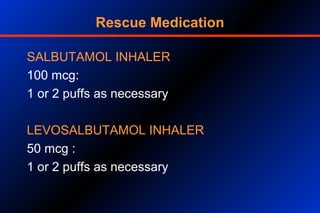
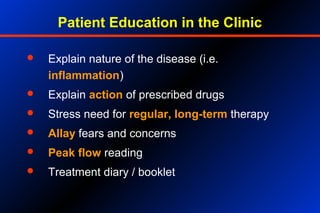
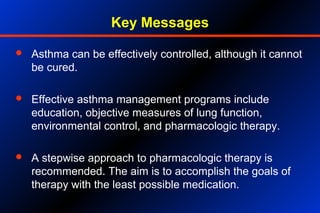
2. Proper diagnosis involves assessing patient history of symptoms, performing a physical exam, and measuring lung function through methods like peak flow meters. Treatment involves a stepwise approach using reliever and preventer medications.
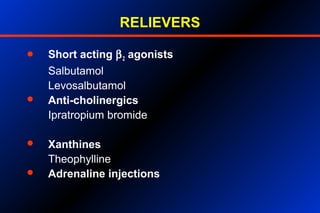
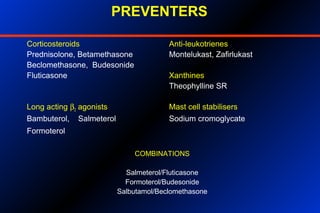
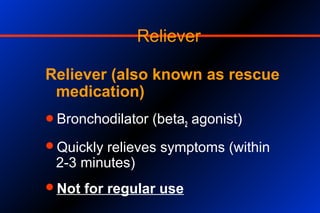
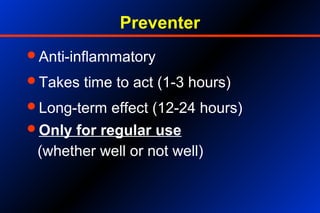
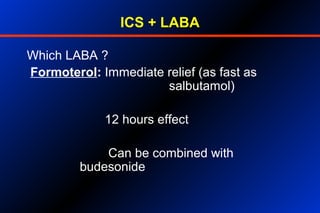
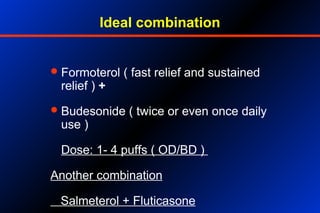
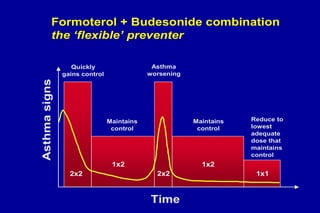
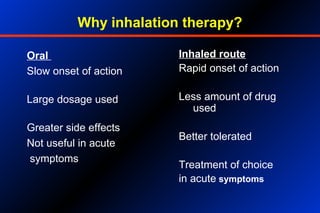
3. Relievers provide quick symptom relief but are not for regular use. Preventers help control inflammation and symptoms over the long-term and include inhaled corticosteroids, long-acting beta-agonists, and other drugs. Combination inhalers containing both a preventer and reliever are often ideal