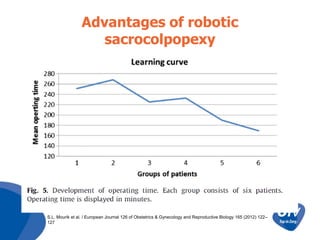
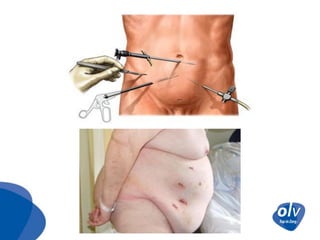
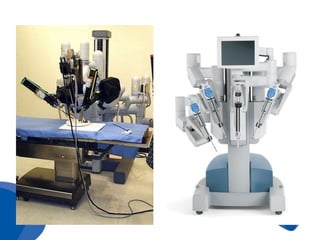
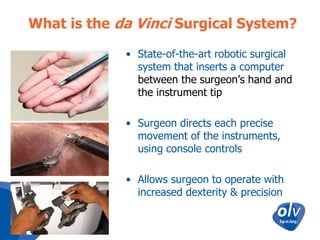
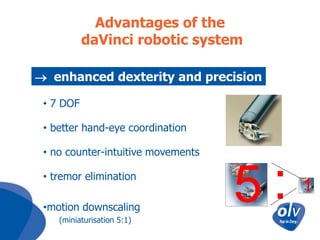
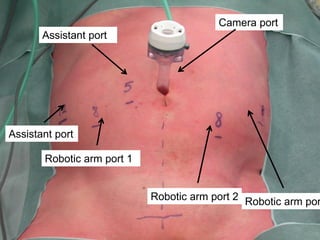
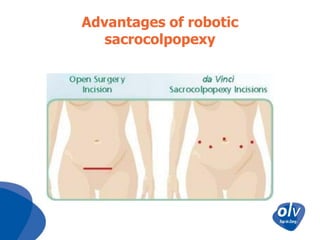
Robotic sacrocolpopexy is a minimally invasive technique for repairing pelvic organ prolapse that provides excellent functional and anatomical results with limited risks. It allows for a complete correction of prolapse in the anterior, posterior, and apical compartments using a single approach. Studies show robotic sacrocolpopexy has comparable outcomes to open surgery with less blood loss and shorter hospital stays. While the technique has a learning curve, it may have advantages over conventional laparoscopy due to its 3D visualization and instrument dexterity.






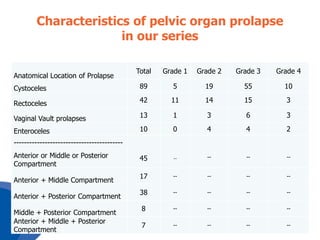
![Demographics, clinical characteristics and frequency
of symptoms at presentation in our series
Age (years)
iBMI
ASA Score
Pelvic heaviness
Urgency
Stress urinary incontinence
Dysuria
Constipation
Urinary tract infection
Median
67
29
1
IQR
[63-73]
[28-32]
[1-2]
No
90
31
%
94.7
32.6
20
21.1
17
12
8
17.9
12.6
8.4](https://image.slidesharecdn.com/roboticsacrocolpopexyolvtechnique-131224050314-phpapp02/85/Robotic-Sacrocolpopexy-OLV-36-320.jpg)