The respiratory system
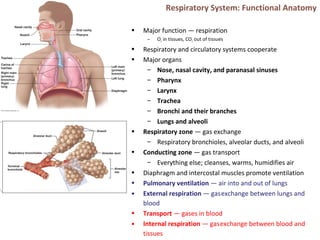
- 1. Respiratory System: Functional Anatomy • Major function — respiration – O2 in tissues, CO2 out of tissues • Respiratory and circulatory systems cooperate • Major organs – Nose, nasal cavity, and paranasal sinuses – Pharynx – Larynx – Trachea – Bronchi and their branches – Lungs and alveoli • Respiratory zone — gas exchange – Respiratory bronchioles, alveolar ducts, and alveoli • Conducting zone — gas transport – Everything else; cleanses, warms, humidifies air • Diaphragm and intercostal muscles promote ventilation • Pulmonary ventilation — air into and out of lungs • External respiration — gasexchange between lungs and blood • Transport — gases in blood • Internal respiration — gasexchange between blood and tissues
- 2. The Nose – Outside • Provides an airway for respiration • Moistens and warms the air • Filters and cleans the air • Resonating chamber for speech • Olfaction • Two regions — external nose and nasal cavity • External nose — root, bridge, dorsum nasi, and apex – Philtrum — shallow vertical groove inferior to apex – Nostrils (nares) — bounded laterally by alae
- 3. The Nose – Inside • Nasal cavity — within and posterior to external nose – Divided by midline nasal septum – Posterior nasal apertures (choanae) open into nasal pharynx – Roof — ethmoid and sphenoid bones – Floor — hard (bone) and soft palates (muscle) • Nasal vestibule — nasal cavity immediately superior to nostrils – Vibrissae (hairs) filter particles • Nasal cavity lined with mucous membranes – Olfactory mucosa • Olfactory epithelium • Respiratory mucosa – Pseudostratified ciliated columnar epithelium – Mucous and serous secretions contain lysozyme and defensins – Cilia move contaminated mucus posteriorly to throat – Inspired air warmed by plexuses of capillaries and veins – Sensory nerve endings trigger sneezing
- 4. Nasal Cavity • Nasal conchae-superior, middle, and inferior – Protrude medially from lateral walls – Increase mucosal area – Enhance air turbulence • Nasal meatus – Groove inferior to each concha • During inhalation, conchae and nasal mucosa – Filter, heat, and moisten air • During exhalation these structures – Reclaim heat and moisture • Paranasal sinuses – In frontal, sphenoid, ethmoid, and maxillary bones – Lighten skull; secrete mucus; help to warm and moisten air • Rhinitis – Inflammation of nasal mucosa – Nasal mucosa continuous with mucosa of respiratory tract spreads from nose throat chest – Spreads to tear ducts and paranasal sinuses causing • Blocked sinus passageways air absorbed vacuum sinus headache
- 5. Pharynx • Muscular tube from base of skull to C6 – Connects nasal cavity and mouth to larynx and esophagus – Composed of skeletal muscle • Three regions • Nasopharynx – Air passageway posterior to nasal cavity – Lining - pseudostratified columnar epithelium – Soft palate and uvula close nasopharynx during swallowing – Pharyngeal tonsil (adenoids) on posterior wall – Pharyngotympanic (auditory) tubes drain and equalize pressure in middle ear; open into lateral walls • Oropharynx – Passageway for food and air from level of soft palate to epiglottis – Lining of stratified squamous epithelium – Isthmus of fauces-opening to oral cavity – Palatine tonsils-in lateral walls of fauces – Lingual tonsil-on posterior surface of tongue • Laryngopharynx – Passageway for food and air – Extends to larynx, where continuous with esophagus – Lined with stratified squamous epithelium
- 6. Larynx • Attaches to hyoid bone; opens into laryngopharynx; continuous with trachea • Functions – Provides patent airway – Routes air and food into proper channels – Voice production • Houses vocal folds • Superior portion–stratified squamous epithelium • Inferior to vocal folds–pseudostratified ciliated columnar epithelium • Nine cartilages of larynx – All hyaline cartilage except epiglottis – Thyroid cartilage with laryngeal prominence (Adam's apple) – Ring-shaped cricoid cartilage – Paired arytenoid, cuneiform, and corniculate cartilages – Epiglottis-elastic cartilage; covers laryngeal inlet during swallowing; covered in taste bud-containing mucosa
- 7. Vocal folds • Vocal ligaments-deep to laryngeal mucosa – Attach arytenoid cartilages to thyroid cartilage – Contain elastic fibers – Form core of vocal folds (true vocal cords) • Glottis-opening between vocal folds • Folds vibrate to produce sound as air rushes up from lungs • Vestibular folds (false vocal cords) – Superior to vocal folds – No part in sound production – Help to close glottis during swallowing • Speech-intermittent release of expired air while opening and closing glottis • Pitch — length and tension of vocal cords • Loudness — force of air • Pharynx, oral, nasal, and sinus cavities amplify and enhance sound • Language — muscles of pharynx, tongue, soft palate, and lips • Vocal folds may act as sphincter to prevent air passage • Example-Valsalva's maneuver – Glottis closes to prevent exhalation – Abdominal muscles contract – Intra-abdominal pressure rises – Emptying rectum or stabilizes trunk
- 8. Trachea • Windpipe–from larynx into mediastinum • Wall composed of three layers – Mucosa-ciliated pseudostratified epithelium with goblet cells – Submucosa-connective tissue with seromucous glands – Adventitia-outermost layer made of connective tissue; encases C-shaped rings of hyaline cartilage • Trachealis muscle – Connects posterior parts of cartilage rings – Contracts during coughing to expel mucus • Carina – Spar of cartilage on last, expanded tracheal cartilage – Point where trachea branches into two main bronchi
- 9. Bronchi and Subdivisions • Air passages undergo 23 orders of branching bronchial (respiratory) tree • From tips of bronchial tree conducting zone structures respiratory zone structures • Trachea → right and left main (primary) bronchi • Each main bronchus enters hilum of one lung – Right main bronchus wider, shorter, more vertical than left • Each main bronchus branches into lobar (secondary) bronchi (three on right, two on left) – Each lobar bronchus supplies one lobe • Each lobar bronchus branches into segmental (tertiary) bronchi – Segmental bronchi divide repeatedly • Branches become smaller and smaller – Bronchioles-less than 1 mm in diameter – Terminal bronchioles-smallest-less than 0.5 mm diameter
- 10. • From bronchi through bronchioles, structural changes occur – Cartilage rings become irregular plates; in bronchioles elastic fibers replace cartilage – Epithelium changes from pseudostratified columnar to cuboidal; cilia and goblet cells become sparse – Relative amount of smooth muscle increases • Allows constriction Respiratory zone • Begins as terminal bronchioles respiratory bronchioles alveolar ducts alveolar sacs – Alveolar sacs contain clusters of alveoli • ~300 million alveoli make up most of lung volume • Sites of gas exchange Conducting and Respiratory Zones
- 11. Respiratory Membrane. Alveoli • Alveolar and capillary walls and their fused basement membranes – ~0.5-µ m-thick; gas exchange across membrane by simple diffusion • Alveolar walls – Single layer of squamous epithelium (type I alveolar cells) • Scattered cuboidal type II alveolar cells secrete surfactant and antimicrobial proteins • Surrounded by fine elastic fibers and pulmonary capillaries • Alveolar pores connect adjacent alveoli • Equalize air pressure throughout lung • Alveolar macrophages keep alveolar surfaces sterile – 2 million dead macrophages/hour carried by cilia throat swallowed
- 12. Alveolar Anatomy
- 13. Lungs • Occupy all thoracic cavity except mediastinum • Root — site of vascular and bronchial attachment to mediastinum • Costal surface — anterior, lateral, and posterior surfaces • Composed primarily of alveoli • Stroma — elastic connective tissue elasticity • Apex-superior tip; deep to clavicle • Base-inferior surface; rests on diaphragm • Hilum-on mediastinal surface; site for entry/exit of blood vessels, bronchi, lymphatic vessels, and nerves • Left lung smaller than right – Cardiac notch-concavity for heart – Separated into superior and inferior lobes by oblique fissure
- 14. Lungs • Right lung – Superior, middle, inferior lobes separated by oblique and horizontal fissures • Bronchopulmonary segments (10 right, 8–10 left) separated by connective tissue septa – If diseased can be individually removed • Lobules-smallest subdivisions visible to naked eye; served by bronchioles and their branches
- 15. Pleurae • Thin, double-layered serosa • Parietal pleura – walls of pleural cavity • Visceral pleura – external lung surface • Pleural fluid fills pleural cavity – Lubrication and surface tension lungs’ expansion and recoil • Pulmonary circulation (low pressure, high volume) – Pulmonary arteries — systemic venous blood to lungs • Branch and feed into pulmonary capillaries – Pulmonary veins — oxygenated blood to the heart • Bronchial arteries — blood to lung tissue – From aorta; enter lungs at hilum – Part of systemic circulation – Supply all lung tissue except alveoli – Bronchial veins anastomose with pulmonary veins
- 16. Mechanics of Breathing. Pressures • Pulmonary ventilation – Inspiration-gases flow into lungs – Expiration-gases exit lungs • Atmospheric pressure (Patm) – Pressure exerted by air surrounding body – 760 mm Hg at sea level = 1 atmosphere • Respiratory pressures – Negative respiratory pressure < Patm – Positive respiratory pressure > Patm – Zero respiratory pressure = Patm • Intrapulmonary (intra-alveolar) pressure (Ppul) – Pressure in alveoli – Fluctuates with breathing – Always eventually equalizes with Patm • Intrapleural pressure (Pip) – Pressure in pleural cavity – Fluctuates with breathing – Always a negative pressure (<Patm and <Ppul) – Fluid level must be minimal • If accumulates positive Pip pressure • Negative Pip caused by – Inward forces → lung collapse • Elastic recoil of lungs ↓ lung size • Surface tension of alveolar fluid ↓ alveolar size – Outward force → enlarge lungs • Elastic chest wall ↑ thorax outward
- 17. Pressure Relationships • If Pip = Ppul or Patm lungs collapse • (Ppul – Pip) = transpulmonary pressure – Keeps airways open – Greater transpulmonary pressure larger lungs • Atelectasis (lung collapse) due to – Plugged bronchioles → collapse of alveoli – Pneumothorax – air in pleural cavity • Rupture in parietal or visceral pleura • Air removed with chest tubes; pleurae heal lung reinflates
- 18. Pulmonary Ventilation. Gas Laws • Inspiration and expiration • Depends on volume changes in thoracic cavity – Volume changes → pressure changes – Pressure changes → gases flow to equalize pressure Boyle’s Law •Relationship between pressure and volume of a gas – Gases fill container; if container size reduced increased pressure •Pressure (P) varies inversely with volume (V): – P1V1 = P2V2
- 19. Inspiration • Active process – Inspiratory muscles (diaphragm and external intercostals) contract – Thoracic volume increases intrapulmonary pressure drops (to −1 mm Hg) – Lungs stretched and intrapulmonary volume increases – Air flows into lungs, down its pressure gradient, until Ppul = Patm • Forced inspiration • Vigorous exercise, COPD accessory muscles (scalenes, sternocleidomastoid, pectoralis minor) further increase in thoracic cage size
- 20. Expiration• Quiet expiration normally passive process – Inspiratory muscles relax – Thoracic cavity volume decreases – Elastic lungs recoil and intrapulmonary volume decreases pressure increases (Ppul rises to +1 mm Hg) – Air flows out of lungs down its pressure gradient until Ppul = 0 • Note: forced expiration-active process; uses abdominal (oblique and transverse) and internal intercostal muscles
- 22. Physical Factors Influencing Pulmonary Ventilation • Three factors hinder air passage and pulmonary ventilation; require energy to overcome • Airway resistance – Friction in airways – major nonelastic source of resistance – F=ΔP/R • ∆P - pressure gradient between atmosphere and alveoli – Resistance usually insignificant • Large airway diameters • Progressive branching of airways ↑ total cross- sectional area • Resistance greatest in medium-sized bronchi – Resistance disappears at terminal bronchioles where diffusion drives gas movement • As airway resistance rises, breathing movements become more strenuous • Severe constriction or obstruction of bronchioles – Can prevent life-sustaining ventilation – Can occur during acute asthma attacks; stops ventilation • Epinephrine dilates bronchioles, reduces air resistance
- 23. • Surfactant – Detergent-like lipid and protein complex produced by type II alveolar cells – ↓ surface tension of alveolar fluid → no alveolar collapse – Insufficient quantity in premature infants causes infant respiratory distress syndrome alveoli collapse after each breath Alveolar Surface Tension • Surface tension – Attracts liquid molecules to one another at gas-liquid interface – Resists any increase of the surface area of liquid – Water – high surface tension; coats alveolar walls reduces them to smallest size
- 24. Lung Compliance • Measure of change in lung volume that occurs with given change in transpulmonary pressure • Higher lung compliance easier to expand lungs • Normally high due to – Distensibility of lung tissue – Alveolar surface tension • Diminished by – Nonelastic scar tissue replacing lung tissue (fibrosis) – Reduced production of surfactant – Decreased flexibility of thoracic cage • Homeostatic imbalances that reduce compliance – Deformities of thorax – Ossification of costal cartilage – Paralysis of intercostal muscles
- 25. Respiratory Volumes and Capacities • Used to assess respiratory status – Tidal volume (TV) – Inspiratory reserve volume (IRV) – Expiratory reserve volume (ERV) – Residual volume (RV) • Combinations of respiratory volumes – Inspiratory capacity (IC) – Functional residual capacity (FRC) – Vital capacity (VC) – Total lung capacity (TLC)
- 26. Dead Space. Pulmonary Function Tests • Anatomical dead space – No contribution to gas exchange – Air remaining in passageways; ~150 ml • Alveolar dead space–non-functional alveoli due to collapse or obstruction • Total dead space-sum of anatomical and alveolar dead space • Spirometer measures respiratory volumes and capacities • Spirometry can distinguish between – Obstructive pulmonary disease—increased airway resistance (e.g., bronchitis) • TLC, FRC, RV ↑ – Restrictive disorders — VC, TLC, FRC, RV ↓ (disease or fibrosis) • To measure rate of gas movement – Forced vital capacity (FVC) — gas forcibly expelled after taking deep breath – Forced expiratory volume (FEV) — amount of gas expelled during specific time intervals of FVC
- 27. Alveolar Ventilation • Minute ventilation-total amount of gas flow into or out of respiratory tract in one minute – Normal at rest = ~ 6 L/min – Normal with exercise = up to 200 L/min – Only rough estimate of respiratory efficiency • Good indicator of effective ventilation • Alveolar ventilation rate (AVR)-flow of gases into and out of alveoli during a particular time • Dead space normally constant • Rapid, shallow breathing decreases AVR AVR = frequency X (TV – dead space) (ml/min) (breaths/min) (ml/breath)
- 28. Nonrespiratory Air Movements • May modify normal respiratory rhythm • Most result from reflex action; some voluntary • Examples include-cough, sneeze, crying, laughing, hiccups, and yawns
- 29. Gas Exchanges – Blood, Lungs, and Tissues • External respiration – diffusion of gases in lungs • Internal respiration – diffusion of gases at body tissues • Both involve – Physical properties of gases – Composition of alveolar gas Dalton’s Law • For mixture of gases: Ptotal = Σ Pindividual • Partial pressure – Pi = k C● i Henry’s Law • Gas mixtures in contact with liquid – Cwater = ks P● i (each gas dissolves in proportion to its partial pressure) – At equilibrium, pressure in both phases equal: • Pwater= Pair – Amount of each gas that will dissolve depends on • Solubility – CO2 20 times more soluble in water than O2; little N2 dissolves in water • Temperature – T ↑, solubility ↓
- 30. Composition of Alveolar Gas • Alveoli contain more CO2 and water vapor than atmospheric air – Gas exchanges in lungs – Humidification of air – Mixing of alveolar gas with each breath
- 31. External Respiration • Exchange of O2 and CO2 across respiratory membrane Influenced by – Thickness and surface area of respiratory membrane • 0.5 to 1 µ m thick • Large total surface area (40 times that of skin) for gas exchange • Thicken if lungs become waterlogged and edematous gas exchange inadequate • Reduced surface area in emphysema (walls of adjacent alveoli break down), tumors, inflammation, mucus
- 32. External Respiration • Exchange of O2 and CO2 across respiratory membrane Influenced by – Partial pressure gradients and gas solubilities • O2 gradient in lungs – Venous blood Po2 = 40 mm Hg – Alveolar Po2 = 104 mm Hg – Oxygen to blood • CO2 gradient in lungs – Venous blood Pco2 = 45 mm Hg – Alveolar Pco2 = 40 mm Hg – CO2 to lungs • Though gradient not as steep, CO2 diffuses in equal amounts with oxygen – CO2 20 times more soluble in plasma than oxygen
- 33. Ventilation-Perfusion Coupling • Exchange of O2 and CO2 across respiratory membrane Influenced by – Ventilation-perfusion coupling • Perfusion-blood flow reaching alveoli • Ventilation-amount of gas reaching alveoli • Ventilation and perfusion matched (coupled) for efficient gas exchange – Never balanced for all alveoli due to • Regional variations due to effect of gravity on blood and air flow • Some alveolar ducts plugged with mucus
- 34. Ventilation-Perfusion Coupling • Perfusion – Changes in Po2 in alveoli cause changes in diameters of arterioles • Where alveolar O2 is high, arterioles dilate • Where alveolar O2 is low, arterioles constrict • Directs most blood where alveolar oxygen high • Changes in Pco2 in alveoli cause changes in diameters of bronchioles – Where alveolar CO2 is high, bronchioles dilate – Where alveolar CO2 is low, bronchioles constrict – Allows elimination of CO2 more rapidly
- 35. Internal Respiration • Capillary gas exchange in body tissues • Partial pressures and diffusion gradients reversed compared to external respiration – Tissue Po2 always lower than in systemic arterial blood oxygen from blood to tissues – CO2 from tissues to blood – Venous blood Po2 40 mm Hg and Pco2 45 mm Hg
- 36. O2 Transport • Molecular O2 carried in blood – 1.5% dissolved in plasma – 98.5% loosely bound to each Fe of hemoglobin (Hb) in RBCs • 4 O2 per Hb • Oxyhemoglobin (HbO2) • Deoxyhemoglobin (HHb – no O2) • Loading and unloading of O2 → change in shape of Hb – As O2 binds, Hb affinity for O2 increases and vice versa – Cooperative binding • All four heme groups carry O2 – full saturation • Rate of loading and unloading of O2 regulated to ensure adequate oxygen delivery to cells – Po2 – Temperature – Blood pH – Pco2 – Concentration of BPG–produced by RBCs during glycolysis; levels rise when oxygen levels chronically low
- 37. Hemoglobin Dissociation Curve • Oxygen-hemoglobin dissociation curve • Hemoglobin saturation plotted against Po2 is S- shaped curve • Binding and release of O2 influenced by Po2
- 38. • In arterial blood – Po2 = 100 mm Hg – Contains 20 ml oxygen per 100 ml blood (20 vol %) – Hb is 98% saturated • Further increases in Po2 (e.g., breathing deeply) produce minimal increases in O2 binding
- 39. • In venous blood – Po2 = 40 mm Hg – Contains 15 vol % oxygen – Hb is 75% saturated • Venous reserve • Oxygen remaining in venous blood
- 40. Factors Influencing Hb Saturation • Increases in temperature, H+ , Pco2, and BPG – Modify structure of hemoglobin; its affinity for O2 ↓ – Occur in systemic capillaries – ↑ O2 unloading from blood – Shift O2-Hb curve to right • Decreases in these factors shift curve to left – Decreases oxygen unloading from blood • As cells metabolize glucose and use O2 – Pco2 and H+ ↑ in capillary blood blood pH ↓, Pco2 ↑ – Heat ↑ Hb affinity for O2 ↓ oxygen unloading ↑ – Bohr effect: oxygen unloading in tissues that use O2 • Hypoxia – Inadequate O2 delivery to tissues cyanosis – Anemic hypoxia–too few RBCs; abnormal or too little Hb – Ischemic hypoxia–impaired/blocked circulation – Histotoxic hypoxia–cells unable to use O2, as in metabolic poisons – Hypoxemic hypoxia–abnormal ventilation; pulmonary disease – Carbon monoxide poisoning–especially from fire; 200X greater affinity for Hb than oxygen
- 41. CO2 Transport • CO2 transported in blood in three forms – 7 to 10% dissolved in plasma – 20% bound to globin of hemoglobin (carbaminohemoglobin) – 70% transported as bicarbonate ions (HCO3 – ) in plasma • CO2 combines with water to form carbonic acid (H2CO3), which quickly dissociates • Occurs primarily in RBCs, where carbonic anhydrase reversibly and rapidly catalyzes reaction
- 42. • In systemic capillaries – HCO3 – quickly diffuses from RBCs into plasma • Chloride shift occurs – Outrush of HCO3 – from RBCs balanced as Cl– moves into RBCs from plasma
- 43. • In pulmonary capillaries – HCO3 – moves into RBCs (while Cl- move out); binds with H+ to form H2CO3 – H2CO3 split by carbonic anhydrase into CO2 and water – CO2 diffuses into alveoli
- 44. Haldane Effect • Amount of CO2 transported affected by Po2 – HHb forms carbaminohemoglobin and buffers H+ more easily – Po2 and hemoglobin saturation ↓; CO2 in blood ↑ • ↑ CO2 exchange in tissues and lungs • At tissues, as more CO2 enters blood – O2 unloading ↑ (Bohr effect) – HbO2 releases O2and readily forms carbaminohemoglobin • Carbonic acid–bicarbonate buffer system–resists changes in blood pH – If H+ concentration in blood rises, excess H+ is removed by combining with HCO3 – H2CO3 – If H+ concentration begins to drop, H2CO3 dissociates, releasing H+ – HCO3 – is alkaline reserve of carbonic acid-bicarbonate buffer system • Changes in respiratory rate and depth affect blood pH – Slow, shallow breathing increased CO2 in blood drop in pH – Rapid, deep breathing decreased CO2 in blood rise in pH
- 45. • Higher brain centers, chemoreceptors, and other reflexes • Neural controls – Neurons in reticular formation of medulla and pons – Clustered neurons in medulla important • Ventral respiratory group • Dorsal respiratory group • Ventral respiratory group (VRG) – Rhythm-generating and integrative center – Sets eupnea (12–15 breaths/minute) • Normal respiratory rate and rhythm – Its inspiratory neurons excite inspiratory muscles via phrenic (diaphragm) and intercostal nerves (external intercostals) – Expiratory neurons inhibit inspiratory neurons • Dorsal respiratory group (DRG) – Near root of cranial nerve IX – Integrates input from peripheral stretch and chemoreceptors; sends information VRG Control of Respiration. Medullary Respiratory Centers
- 46. Pontine Respiratory Centers • Influence and modify activity of VRG • Smooth out transition between inspiration and expiration and vice versa • Transmit impulses to VRG modify and fine- tune breathing rhythms during vocalization, sleep, exercise Respiratory Rhythm •Not well understood •One hypothesis – Pacemaker neurons with intrinsic rhythmicity •Most widely accepted hypothesis – Reciprocal inhibition of two sets of interconnected pacemaker neurons in medulla that generate rhythm
- 47. Factors influencing Breathing Rate and Depth • Depth determined by how actively respiratory center stimulates respiratory muscles • Rate determined by how long inspiratory center active • Both modified in response to changing body demands – Most important are changing levels of CO2, O2, and H+ – Sensed by central and peripheral chemoreceptors
- 48. Chemical Factors • Influence of Pco2 (most potent; most closely controlled) – blood Pco2 levels ↑ (hypercapnia), CO2 accumulates in brain – CO2 in brain hydrated carbonic acid dissociates, releasing H+ pH ↓ – H+ stimulates central chemoreceptors of brain stem – Chemoreceptors synapse with respiratory regulatory centers depth and rate of breathing ↑ blood Pco2 ↓ pH ↑ • Hyperventilation –depth/rate of breathing ↑; exceeds body's need to remove CO2 blood CO2 levels ↓ (hypocapnia) cerebral vasoconstriction and cerebral ischemia dizziness, fainting • Apnea – breathing cessation from abnormally low Pco2
- 49. Chemical Factors • Influence of Po2 – Peripheral chemoreceptors in aortic and carotid bodies – arterial O2 level sensors • When excited, cause respiratory centers to increase ventilation – ↓ Po2 – normally slight effect on ventilation • O2 reservoir in HbO2 • Requires substantial drop in arterial Po2 (to 60 mm Hg) to stimulate increased ventilation • Influence of arterial pH – Can modify respiratory rate and rhythm even if CO2 and O2 levels normal – Mediated by peripheral chemoreceptors – ↓ pH may reflect • CO2 retention; accumulation of lactic acid; excess ketone bodies – Respiratory system controls ↑ pH by ↑ respiratory rate and depth • ↑CO2 levels most powerful respiratory stimulant • Normally blood Po2 affects breathing only indirectly by influencing peripheral chemoreceptor sensitivity to changes in Pco2 • When arterial Po2 falls below 60 mm Hg, it becomes major stimulus for respiration (via peripheral chemoreceptors) • Changes in arterial pH resulting from CO2 retention or metabolic factors act indirectly through peripheral chemoreceptors
- 50. Influence of Higher Brain Centers • Hypothalamic controls act through limbic system to modify rate and depth of respiration – Example-breath holding that occurs in anger or gasping with pain • Rise in body temperature increases respiratory rate • Cortical controls-direct signals from cerebral motor cortex that bypass medullary controls – Example-voluntary breath holding • Brain stem reinstates breathing when blood CO2 critical
- 51. Inflation Reflex • Hering-Breuer Reflex (inflation reflex) – Stretch receptors in pleurae and airways stimulated by lung inflation • Inhibitory signals to medullary respiratory centers end inhalation and allow expiration • Acts as protective response more than normal regulatory mechanism Pulmonary Irritant Reflexes • Receptors in bronchioles respond to irritants – Communicate with respiratory centers via vagal nerve afferents • Promote reflexive constriction of air passages • Same irritant cough in trachea or bronchi; sneeze in nasal cavity
- 52. Respiratory Adjustments: Exercise and High Altitude • Adjustments geared to both intensity and duration of exercise • Hyperpnea – ↑ ventilation (10 to 20 fold) • Pco2, Po2, and pH remain during exercise≡ • Three neural factors cause increase in ventilation as exercise begins – Psychological stimuli – Simultaneous cortical motor activation of skeletal muscles and respiratory centers – Excitatory impulses to respiratory centers from proprioceptors • Ventilation declines suddenly as exercise ends because the three neural factors shut off • Gradual decline to baseline because of decline in CO2 flow after exercise ends • Exercise anaerobic respiration lactic acid – Not from poor respiratory function; from insufficient cardiac output or skeletal muscle inability to increase oxygen uptake • Quick travel to altitudes above 2400 meters (8000 feet) may symptoms of acute mountain sickness (AMS) – Atmospheric pressure and Po2 levels ↓ – Headaches, shortness of breath, nausea, and dizziness – (Lethal) cerebral and pulmonary edema • Acclimatization-respiratory and hematopoietic adjustments to high altitude – Chemoreceptors – more responsive to Pco2 when Po2 ↓ – ↓ in Po2 directly stimulates peripheral chemoreceptors – Minute ventilation ↑ and stabilizes in few days to 2–3 L/min higher than at sea level • Always lower-than-normal Hb saturation levels – Less O2 available • ↓ blood O2 → ↑ production of EPO in kidneys • RBC ↑ slowly → long-term compensation
- 53. COPD. Emphysema • Chronic obstructive pulmonary disease (COPD) – Exemplified by chronic bronchitis and emphysema – Irreversible decrease in ability to force air out of lungs – Other common features • History of smoking in 80% of patients • Dyspnea - labored breathing ("air hunger") • Coughing and frequent pulmonary infections • Most develop respiratory failure (hypoventilation) accompanied by respiratory acidosis, hypoxemia • Emphysema – Permanent enlargement of alveoli; destruction of alveolar walls; decreased lung elasticity • Accessory muscles necessary for breathing exhaustion from energy usage • Hyperinflation flattened diaphragm reduced ventilation efficiency • Damaged pulmonary capillaries enlarged right ventricle
- 54. Homeostatic Imbalance • Chronic bronchitis – Inhaled irritants chronic excessive mucus inflamed and fibrosed lower respiratory passageways obstructed airways impaired lung ventilation and gas exchange frequent pulmonary infections • COPD symptoms and treatment – Strength of innate respiratory drive different symptoms in patients • "Pink puffers"–thin; near-normal blood gases • "Blue bloaters"–stocky, hypoxic – Treated with bronchodilators, corticosteroids, oxygen, sometimes surgery • Asthma – reversible COPD – Characterized by coughing, dyspnea, wheezing, and chest tightness – Active inflammation of airways precedes bronchospasms – Airway inflammation is immune response caused by release of interleukins, production of IgE, and recruitment of inflammatory cells – Airways thickened with inflammatory exudate magnify effect of bronchospasms
- 55. Tuberculosis. Lung Cancer. • Tuberculosis (TB) – Infectious disease caused by bacterium Mycobacterium tuberculosis – Symptoms-fever, night sweats, weight loss, racking cough, coughing up blood – Treatment- 12-month course of antibiotics • Are antibiotic resistant strains • Lung cancer – Leading cause of cancer deaths in North America – 90% of all cases result of smoking – Three most common types • Adenocarcinoma (~40% of cases) peripheral lung areas (bronchial glands, alveolar cells) • Squamous cell carcinoma (20–40% of cases) in bronchial epithelium • Small cell carcinoma (~20% of cases) - lymphocyte-like cells; originate in primary bronchi; metastasize http://www.lung.org/
- 56. Lung Cancer • Lung cancer – Early detection key to survival – Helical CT scan better than chest X ray – Developing breath test of gold nanoparticles – If no metastasis surgery to remove diseased lung tissue – If metastasis radiation and chemotherapy • Potential new therapies for lung cancer – Antibodies targeting growth factors required by tumor; or deliver toxic agents to tumor – Cancer vaccines to stimulate immune system – Gene therapy to replace defective genes http://www.aboutcancer.com/
- 57. Early Development • Upper respiratory structures develop first • Olfactory placodes invaginate into olfactory pits ( nasal cavities) by fourth week • Laryngotracheal bud present by fifth week • Mucosae of bronchi and lung alveoli present by eighth week • By 28th week, premature baby can breathe on its own • During fetal life, lungs filled with fluid and blood bypasses lungs • Gas exchange takes place via placenta
- 58. Age and Respiratory System • At birth, respiratory centers activated, alveoli inflate, and lungs begin to function • Two weeks after birth before lungs fully inflated • Respiratory rate highest in newborns and slows until adulthood • Lungs continue to mature and more alveoli formed until young adulthood • Respiratory efficiency decreases in old age http://www.nursingconsult.com/
- 59. Cystic Fibrosis • Cystic fibrosis – Most common lethal genetic disease in North America – Abnormal, viscous mucus clogs passageways bacterial infections • Affects lungs, pancreatic ducts, reproductive ducts – Cause–abnormal gene for Cl- membrane channel http://learn.genetics.utah.edu/http://www.nhlbi.nih.gov/ • Treatments for cystic fibrosis – Mucus-dissolving drugs; chest percussion to loosen mucus; antibiotics – Research into • Introducing normal genes • Prodding different protein Cl- channel • Freeing patient's abnormal protein from ER to Cl- channels • Inhaling hypertonic saline to thin mucus