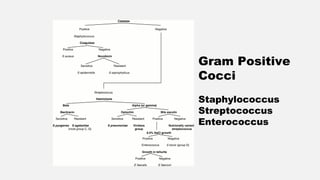
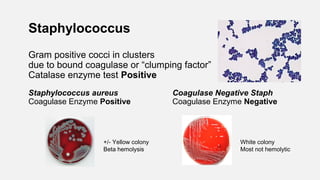
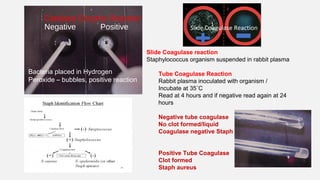
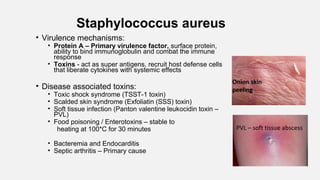
This document provides an overview of bacteriology concepts and procedures. It defines different types of bacteria based on oxygen requirements and discusses specimen collection and transport methods. Procedures like gram staining and MALDI-TOF mass spectrometry for bacterial identification are summarized. Common gram positive cocci like Staphylococcus, Streptococcus, and Enterococcus are discussed in terms of identification and pathogenic species.
![Streptococcus pyogenes
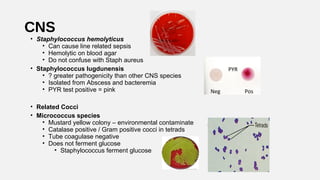
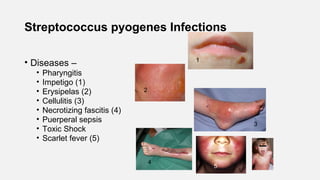
• Group A beta Streptococcus [GAS]
• Bacitracin KB sensitivity test – inhibited, no growth @ disk
• This test is not specific for Group A , it x-reacts with group C
• PYR (pyrrolidonyl arylmidase) reaction
• Organism spotted onto moist PYR disk
• 2 min – RT incubation
• Add Cinnamaldehyde reagent
• Pink = positive = Strep pyogenes
• This test is not exclusive for Strep pyogenes –
Enterococcus and Staph lugdunensis also (+)
• Therapy : Penicillin or Cephalosporin antibiotics
No resistance reported to these agents
PYR](https://image.slidesharecdn.com/margiemorgan-webbacteriologyupdate2019-190331040436/85/Bacteriology-Update-2019-21-320.jpg)
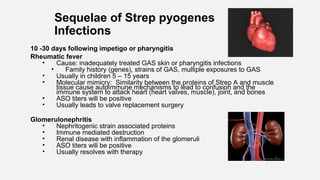
![Strep agalactiae [GBS]
• Pathogen of the elderly – Bacteremia and urinary tract infection
• Pathogen of neonate bacteremia or CNS – in utero or perinatal organism acquisition
during birthing process, infection in @ 1/2000 births
• Early onset – within 7 days
• Late 7 – 28 days from birth process.
• Treatment: Penicillin or Cephalosporin (3rd
generation)
• Pregnant women colonized in the cervix and/or rectal area (@25%)
• All pregnant must be tested at 35 – 37 weeks of pregnancy.
• Enrichment methods for GBS are standard of practice and must be
used
• Swab incubated in enrichment broth (LIM) for 18 hours at 35 ˚C then subcultured onto
Blood agar. Enrichment broth can also be used in molecular testing methods
• Ampicillin drug of choice for prevention of neonatal infection
• Susceptibility testing for alternative therapies
• Clindamycin testing with Inducible resistance testing confirmation](https://image.slidesharecdn.com/margiemorgan-webbacteriologyupdate2019-190331040436/85/Bacteriology-Update-2019-26-320.jpg)

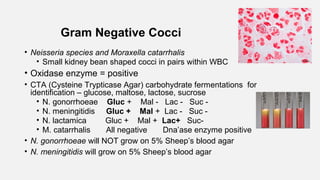
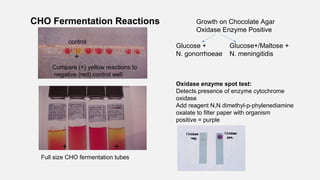
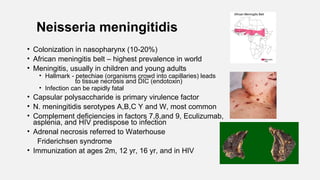
![Neisseria gonorrhoeae
• STD - acute urethritis, endocervix, ocular, rectal, oropharynx, septic arthritis
• 10-20 % female ascend to PID but only 0.5% disseminate
• Gram stain of urethral discharge useful/specific for male diagnosis
• Gram stain of cervix can be problematic due to NF look alike organisms, primarily
Acinetobacter species
• Transport for culture – charcoal swabs at room temperature
• Media: Selective Thayer Martin or Martin Lewis agar, chocolate type agar with
antibiotics
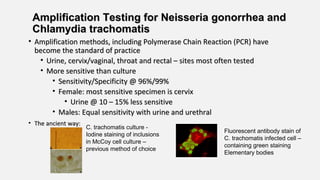
• Amplification methods [PCR] are standard of practice, improved sensitivity
comparted to culture methods
• Has both a beta lactamase enzyme and Chromosomal resistance mechanisms:
• Therapy: Ceftriaxone + Azithromycin or Doxycycline, combination therapy to
prevent development of resistance](https://image.slidesharecdn.com/margiemorgan-webbacteriologyupdate2019-190331040436/85/Bacteriology-Update-2019-40-320.jpg)

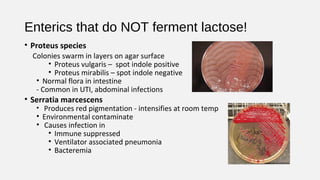
![• Escherichia coli
• Normal flora in human intestine
• #1 cause of UTI [@80%]
• Also, bacteremia, neonatal meningitis,
and abdominal infections
• Ferments lactose when grown on MacConkey agar
• Spot indole reaction = positive
• Detects breakdown of tryptophan from growth on blood agar
• Green sheen produced when grown on Eosin methylene blue agar
• Pathogen of diarrhea
• Enterotoxigenic (ETEC) E. coli is the cause of traveler’s diarrhea
• Enterohemorrhagic E. coli (EHEC) (such as 0157:H7)
• Bloody diarrhea acquired from eating undercooked meat from an infected
cow – pathogenicity from Shiga toxin production
• Hemolytic uremic syndrome (HUS) can result [hemolytic anemia,
thrombocytopenia, and renal failure] particularly in young children
• When grown on MAC agar with sorbitol / does NOT ferment sorbitol
Green sheen on
EMB agar
Indole positive
Lactose
fermentor](https://image.slidesharecdn.com/margiemorgan-webbacteriologyupdate2019-190331040436/85/Bacteriology-Update-2019-53-320.jpg)
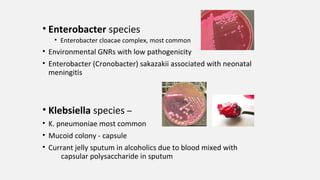
![Glu/lac/suc
fermented
with gas
Glucose
fermented
Glucose
fermented
with H2S
No CHO
fermentation
Non fermenter
Triple Sugar Iron Agar (TSI)– Used to detect
fermentation of glucose, lactose and/or sucrose and
production of hydrogen sulfide [H2S]
Fermentation= yellow medium
Gas = Disruption of the agar
H2S
No fermentation =
Red medium](https://image.slidesharecdn.com/margiemorgan-webbacteriologyupdate2019-190331040436/85/Bacteriology-Update-2019-56-320.jpg)
![• Salmonella species
• Diarrhea with +/- fever – polys in the stool
• Infection from eating contaminated food (raw eggs)or directly from
contact with a sick animal
– must ingest large #’s of organisms to make you ill (1,00,000 bacteria),
stomach acid is protective
• Does not ferment lactose
• Produces Hydrogen sulfide on TSI slant and selective agars
• Motile
• Identification based on biochemical reactions and serologic typing
• Kaufman White serologic typing for speciation of Salmonella
• O Somatic (cell wall) antigen – Salmonella group “B”
• H flagellar antigens – 2 phases [h1 & h2]
• Vi capsular antigen – Salmonella typhi only](https://image.slidesharecdn.com/margiemorgan-webbacteriologyupdate2019-190331040436/85/Bacteriology-Update-2019-57-320.jpg)
![Shigella
• Diarrhea, +/-vomiting, fluid loss, polys and blood in stool
• Infection : Human to human transmission /control with good
hygiene
• Low #’s of organisms make you ill [10 – 100 bacteria]
• Does not ferment lactose
• Non motile
• No H2S produced
• 4 species based on somatic antigen
• S. boydii Group C
• S. dysenteriae Group A
• S. flexneri Group B
• S. sonnei Group D](https://image.slidesharecdn.com/margiemorgan-webbacteriologyupdate2019-190331040436/85/Bacteriology-Update-2019-59-320.jpg)
![Salmonella Shigella Agar (SS
agar)
Salmonella and Shigella are colorless
due to lactose not being fermented –
H2S produced by Salmonella turning
colony black
Hektoen agar –
Salmonella produces H2S [Hydrogen sulfide]
producing black colonies
Shigella – green colonies
Normal flora – orange colored due to
fermentation of lactose (E. coli)
Non-Lactose fermenter
Shigella
Salmonella
Normal Flora
Lactose fermented
H2S](https://image.slidesharecdn.com/margiemorgan-webbacteriologyupdate2019-190331040436/85/Bacteriology-Update-2019-60-320.jpg)

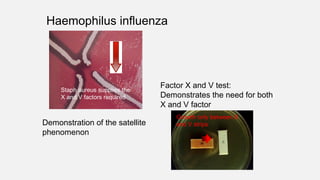
![Haemophilus influenzae
• Transmission – close contact/secretions
• Virulence factor – capsular polysaccharide
• Small pleomorphic Gram negative rod
• Requires 2 nutritional factors for growth:
• X factor = hemin
• V factor = NAD (nicotinamide adenine dinucleotide)
• Grows on chocolate agar (has X and V factor)
• Will not grow on 5% sheep’s blood agar
• Requires C0₂ [5 – 8%] for growth
• Effective vaccine targets invasive infections with H. influenzae type B (HIB)
– effectively eliminating most childhood invasive infections
• Resistance to Ampicillin due to beta lactamase enzyme productions [25
%], 3rd
generation Cephalosporin becomes the antibiotic of choice
(Ceftriaxone) for invasive infections](https://image.slidesharecdn.com/margiemorgan-webbacteriologyupdate2019-190331040436/85/Bacteriology-Update-2019-69-320.jpg)
![• C. septicum –
• Bacteremia or Gas Gangrene in patient with underlying
malignancy
• Hematogenous spread from GI tract – no trauma necessary
• C. difficile –
• Disease: antibiotic associated colitis, pseudomembranous
colitis from toxin production
• Toxin A – enterotoxin causing fluid accumulation
• Toxin B – potent cell cytotoxin – primary virulence
• Binary toxin – so called Nap1 strain is produces larger amount of
toxin
• Diagnosis of infection:
• EIA methods [toxin A/B] are insensitive but detect active toxin
• PCR methods [toxin A/B] are more sensitive, detect toxin genes
• Culture – Cycloserine, Cefoxitin, Fructose Agar [CCFA]
• Infants have @ 70% colonization rate – do not test](https://image.slidesharecdn.com/margiemorgan-webbacteriologyupdate2019-190331040436/85/Bacteriology-Update-2019-97-320.jpg)