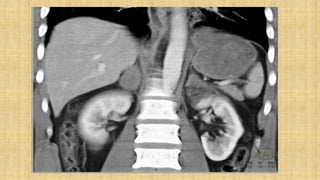
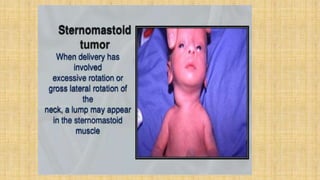
The document discusses various types of birth injuries including:
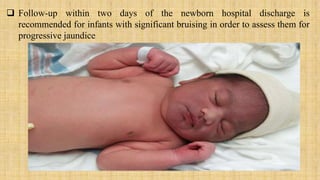
1. Soft tissue injuries such as bruising, petechiae, and subcutaneous fat necrosis.
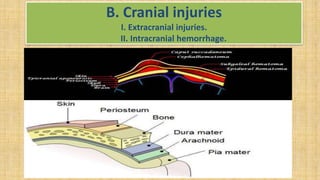
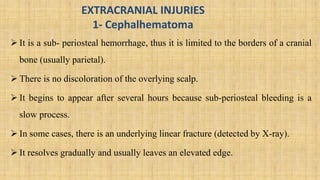
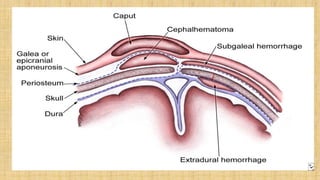
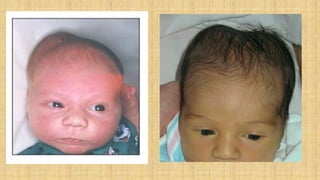
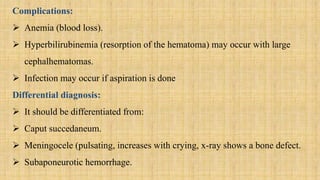
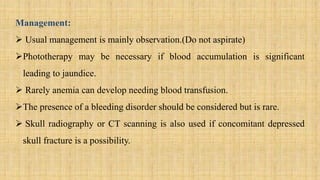
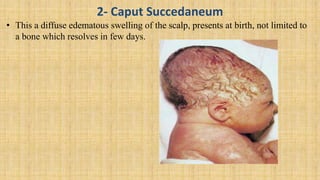
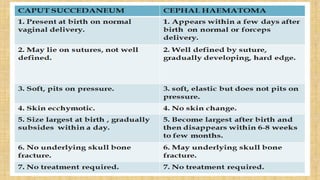
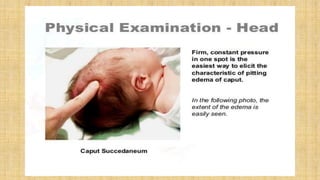
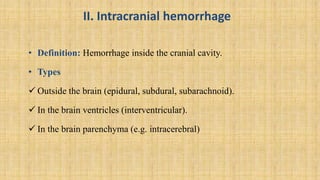
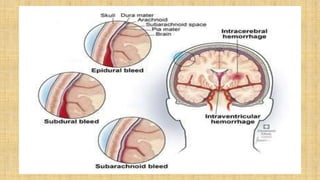
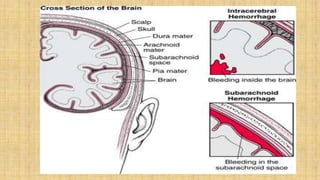
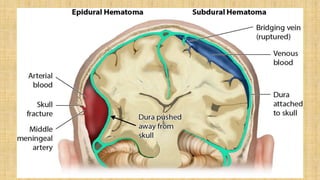
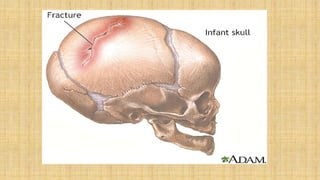
2. Cranial injuries including cephalhematoma, caput succedaneum, subaponeurotic hemorrhage, and intracranial hemorrhage.
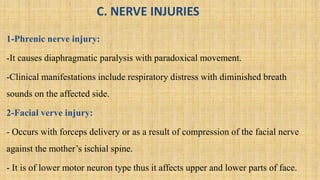
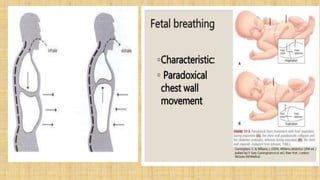
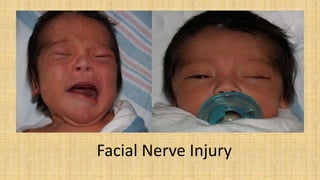
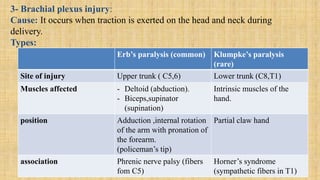
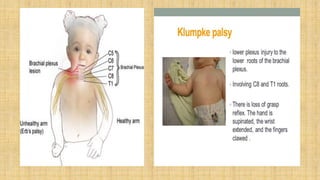
3. Nerve injuries like phrenic nerve injury and brachial plexus injury.
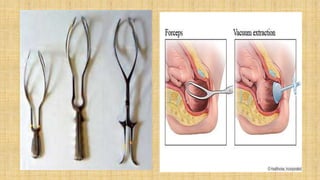
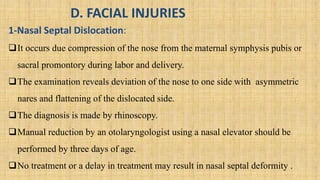
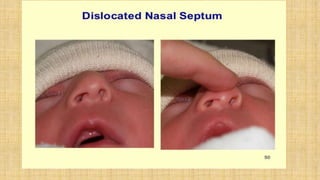
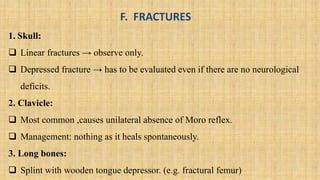
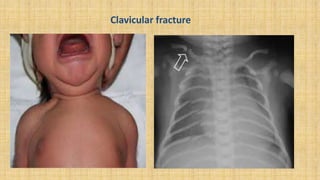
It also covers facial injuries, visceral injuries, fractures, and dislocations that can occur during birth along with their causes, presentations, and treatments. Risk factors for birth injuries include large baby size, instrumental delivery, and abnormal fetal positioning.