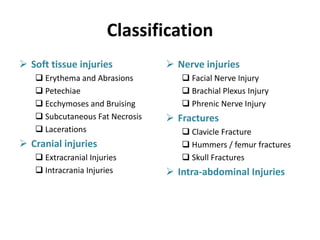
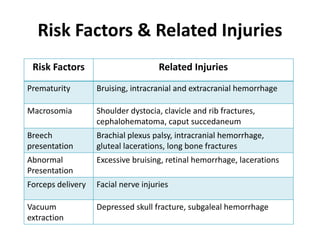
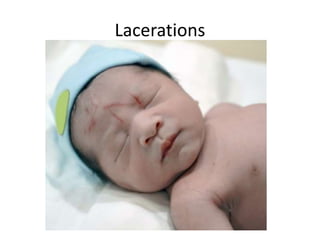
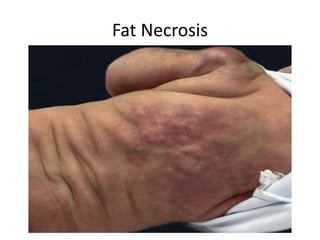
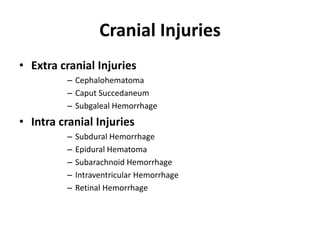
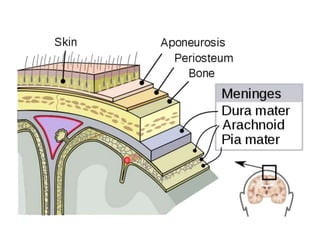
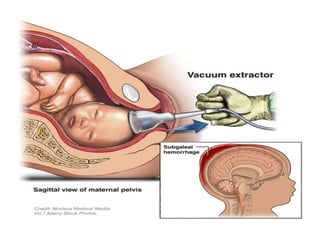
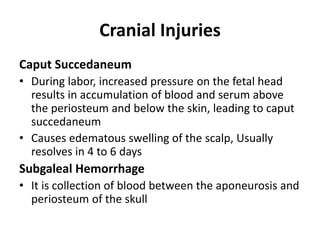
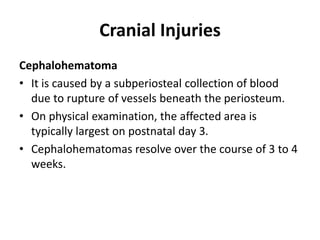
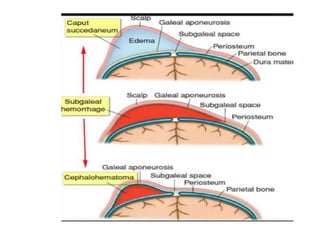
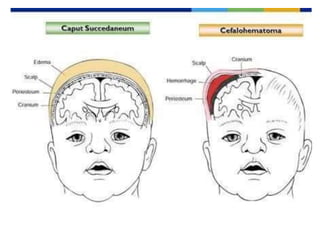
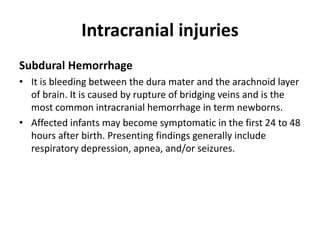
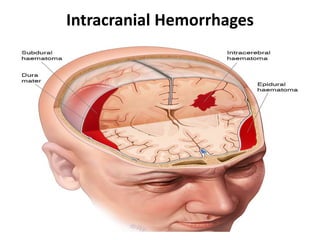
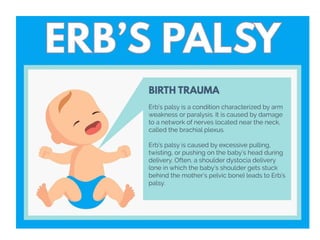
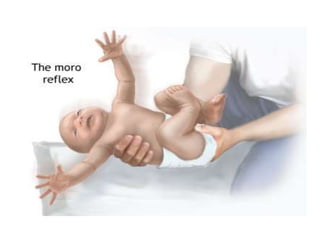
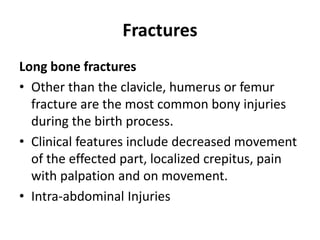
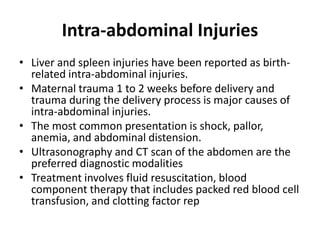
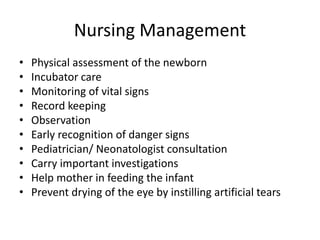
This document discusses various types of birth injuries that can occur in newborns, including soft tissue injuries, cranial injuries, nerve injuries, fractures, and intra-abdominal injuries. It identifies risk factors for birth injuries such as prematurity, large baby size, breech presentation, and traumatic delivery methods. Each type of injury is defined and examples are provided, along with typical signs, symptoms, and treatment approaches. Nursing management focuses on close physical assessment, monitoring, consultation, and supporting feeding when appropriate.