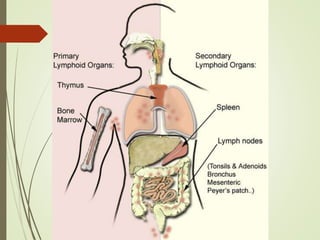
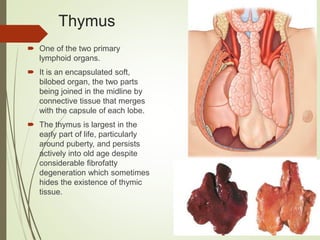
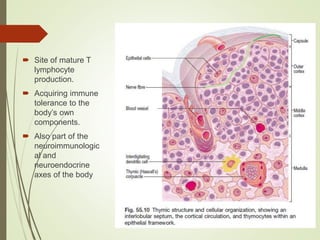
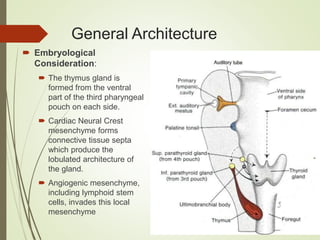
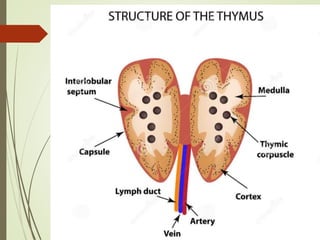
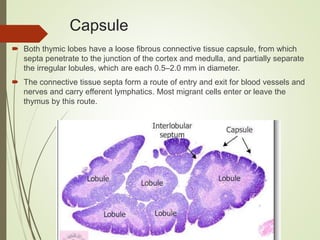
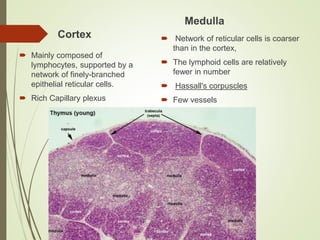
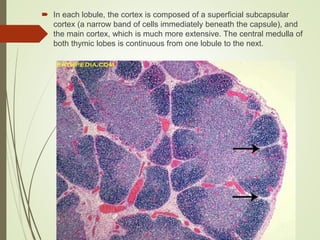
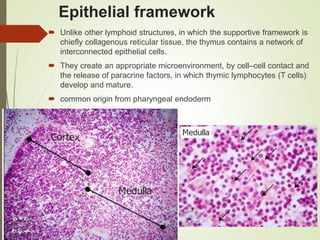
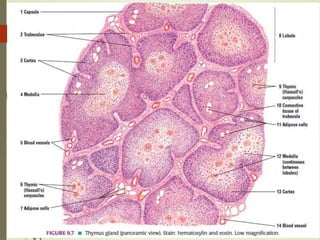
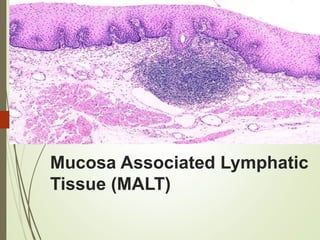
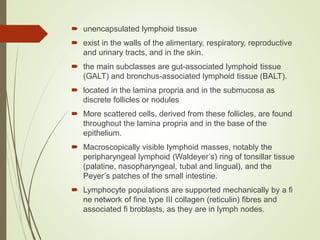
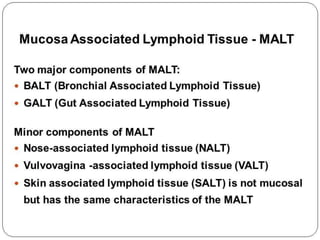
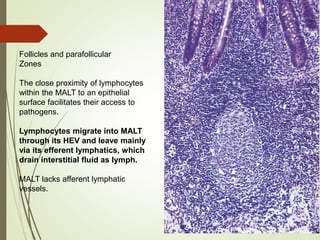
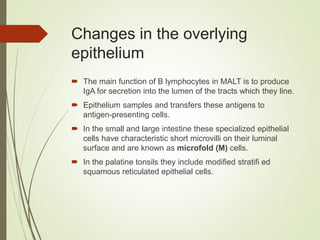
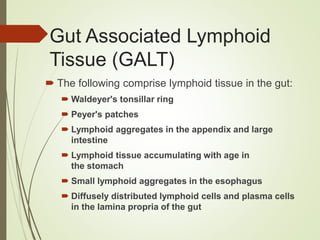
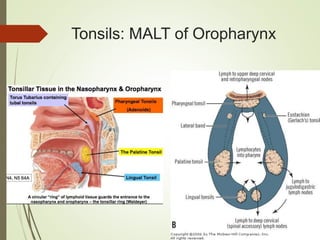
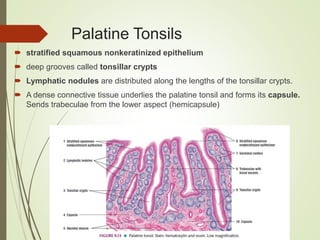
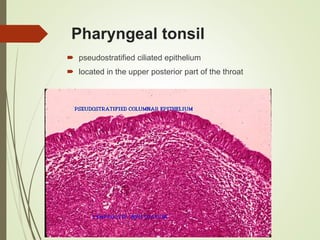
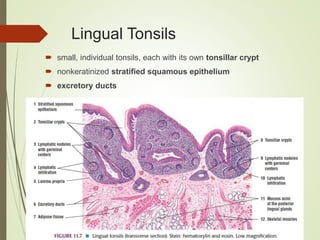
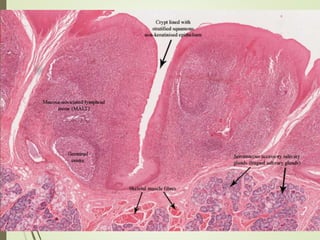
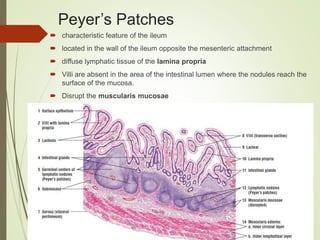
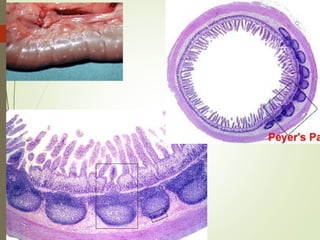
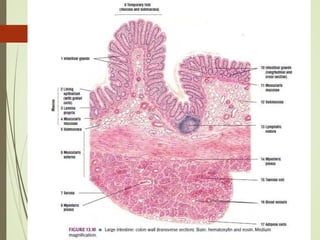
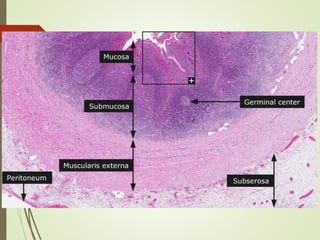
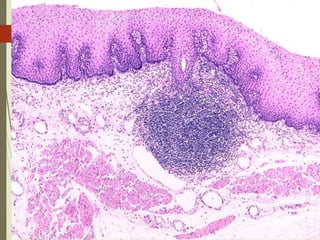
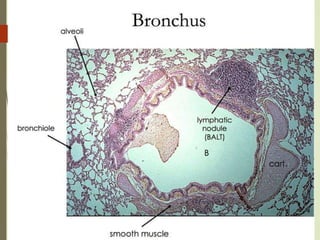
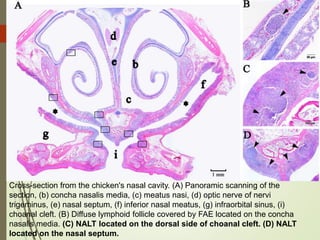
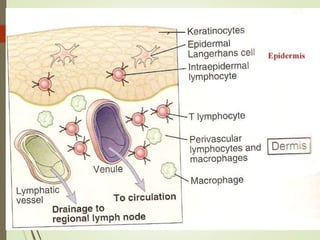
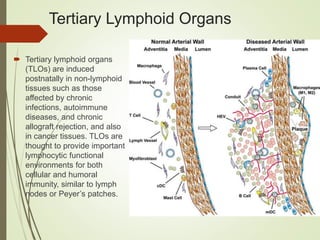
The document discusses various lymphatic tissues in the body, including the thymus, tonsils, mucosa-associated lymphoid tissue (MALT), and tertiary lymphoid organs. It describes the microanatomy and functions of the thymus, tonsils, Peyer's patches in the small intestine, and nasal-associated lymphoid tissue. It also explains that tertiary lymphoid organs can develop in non-lymphoid tissues affected by chronic conditions to provide immune responses.