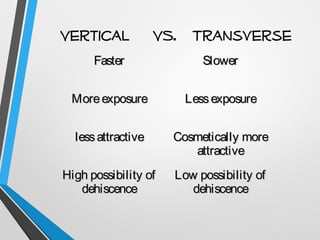
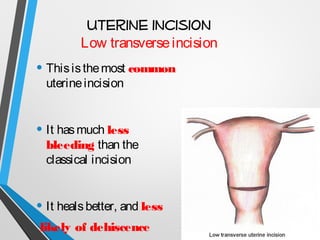
This document provides an overview of the key steps in a Cesarean section (CS) procedure. It discusses preoperative preparation including positioning the patient on their left side. It describes spinal or general anesthesia options. The surgical technique involves making a vertical or transverse abdominal incision and then a low transverse uterine incision. The infant is gently delivered and the cord is clamped. The placenta is then manually removed if not delivered spontaneously. The uterine incision is closed with absorbable sutures. In some cases a hysterectomy may be required as part of the procedure due to complications.