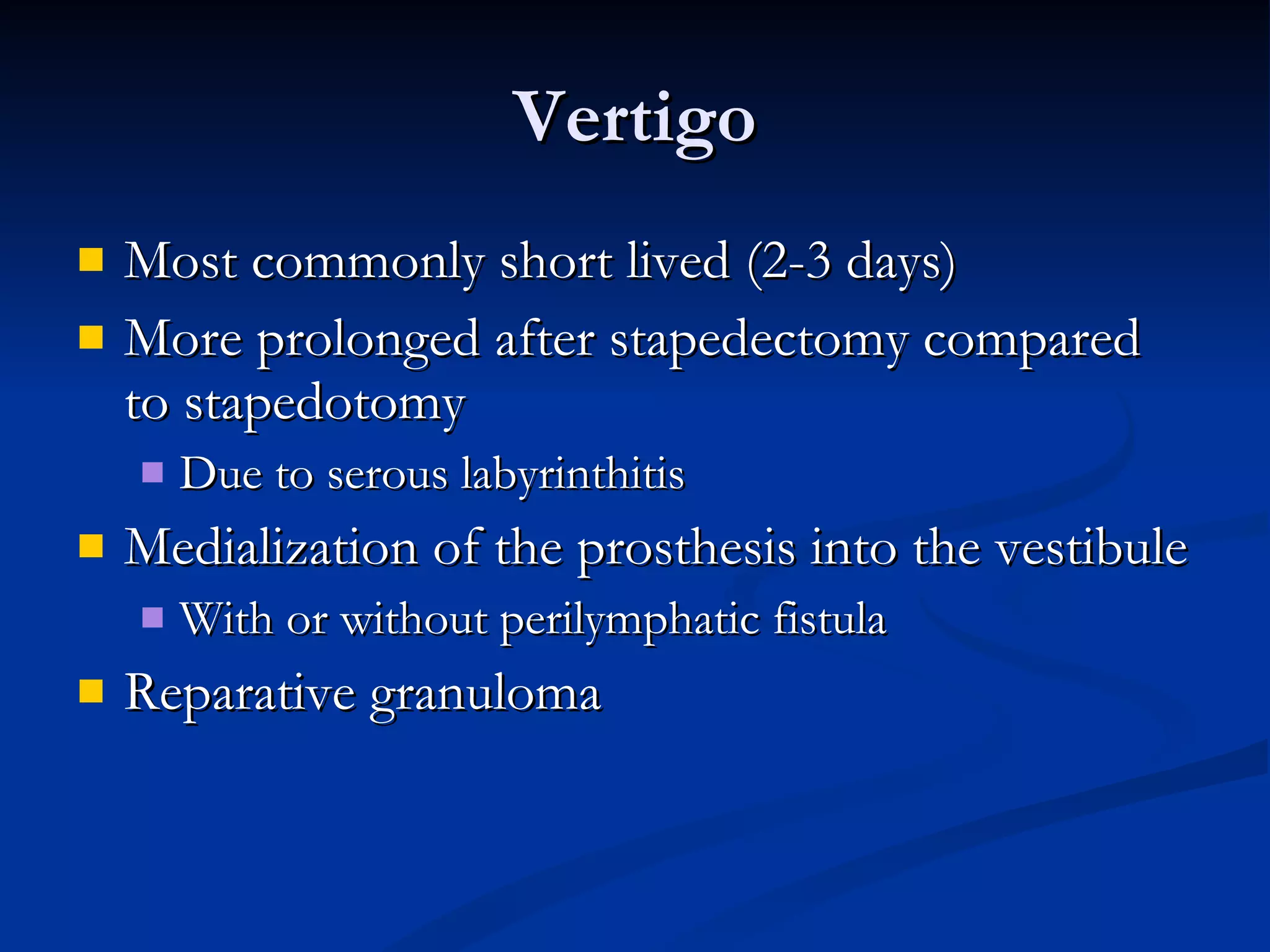
The document discusses otosclerosis, a primary metabolic bone disease that results in fixation of the ossicles and conductive hearing loss. It provides a historical overview of otosclerosis and stapes surgery, details the epidemiology and pathophysiology of otosclerosis, and describes the diagnostic evaluation, medical and surgical management options for treating otosclerosis. The surgical procedure of stapedectomy and potential complications are also outlined.