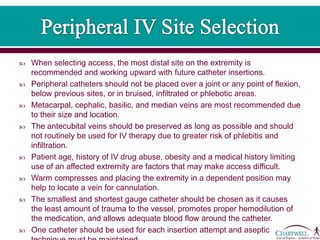
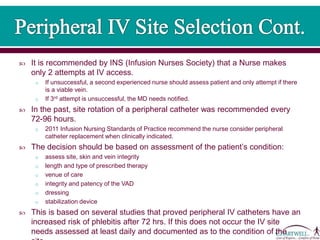
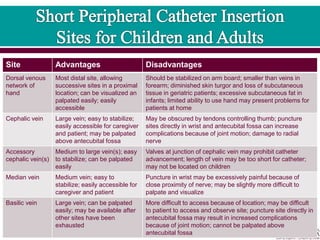
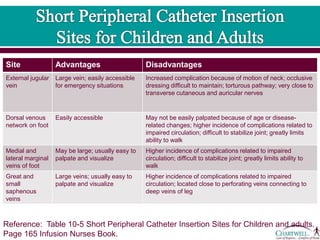
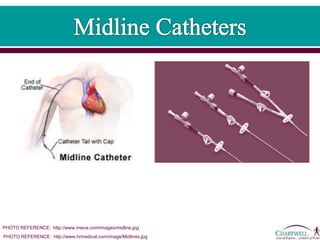
This document discusses peripheral and midline intravenous catheters. It notes that peripheral catheters are appropriate for short term therapies under 7 days through superficial hand or arm veins. Midline catheters are inserted further up the arm and can remain in place for 1-4 weeks, providing less frequent site changes than peripheral catheters. The document reviews best practices for catheter insertion, stabilization, dressing, and flushing to promote safe and effective venous access.