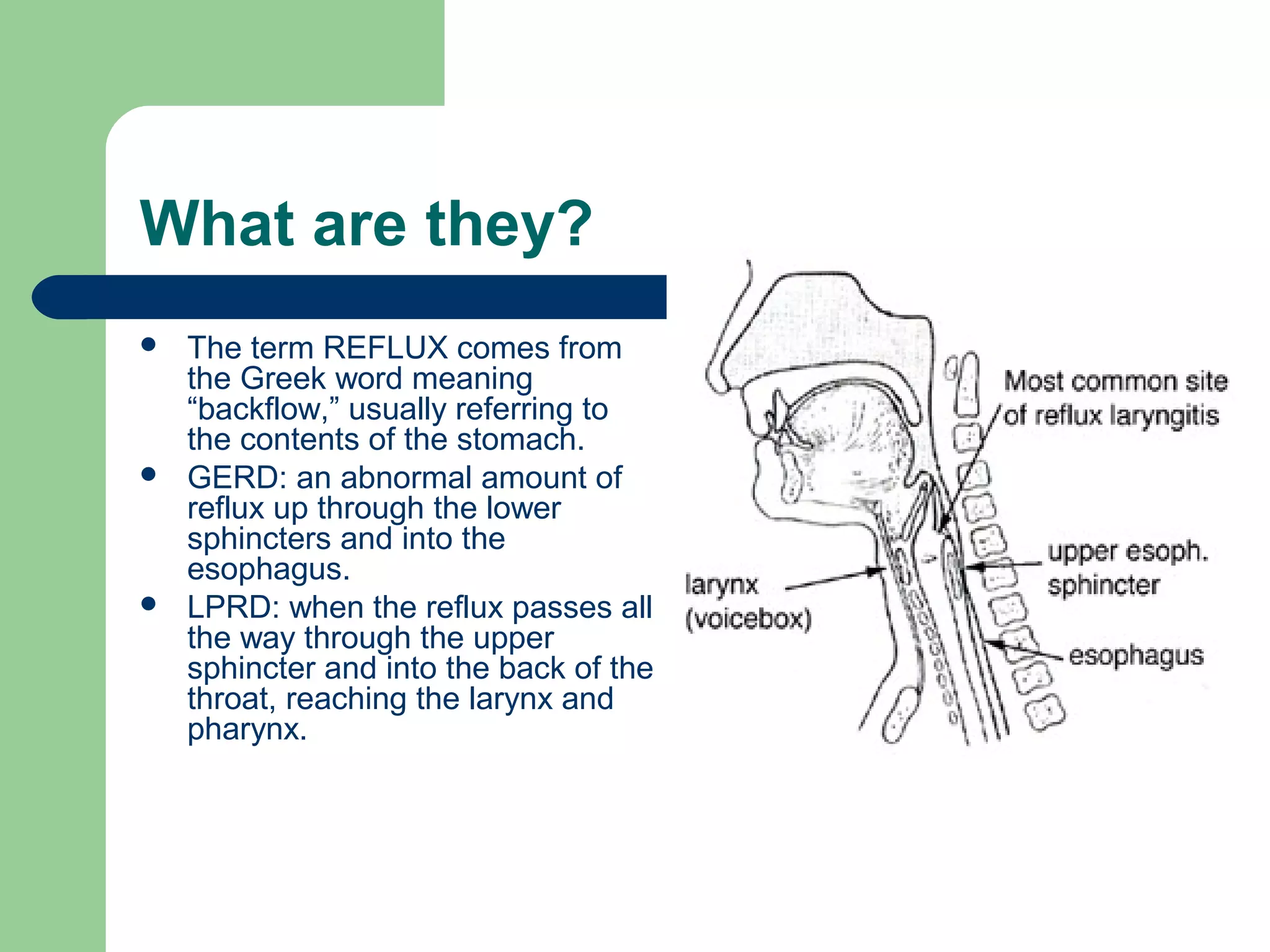
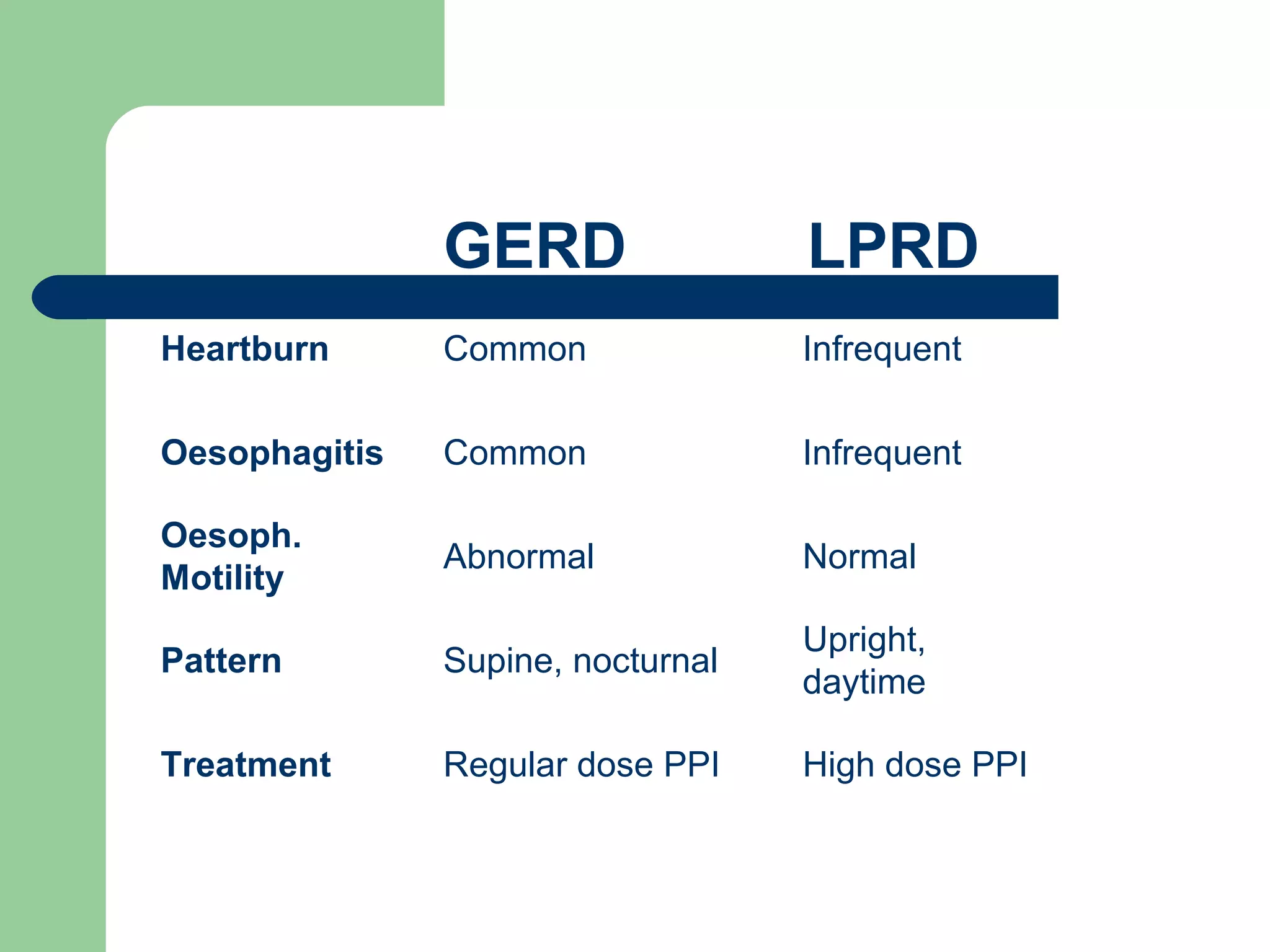
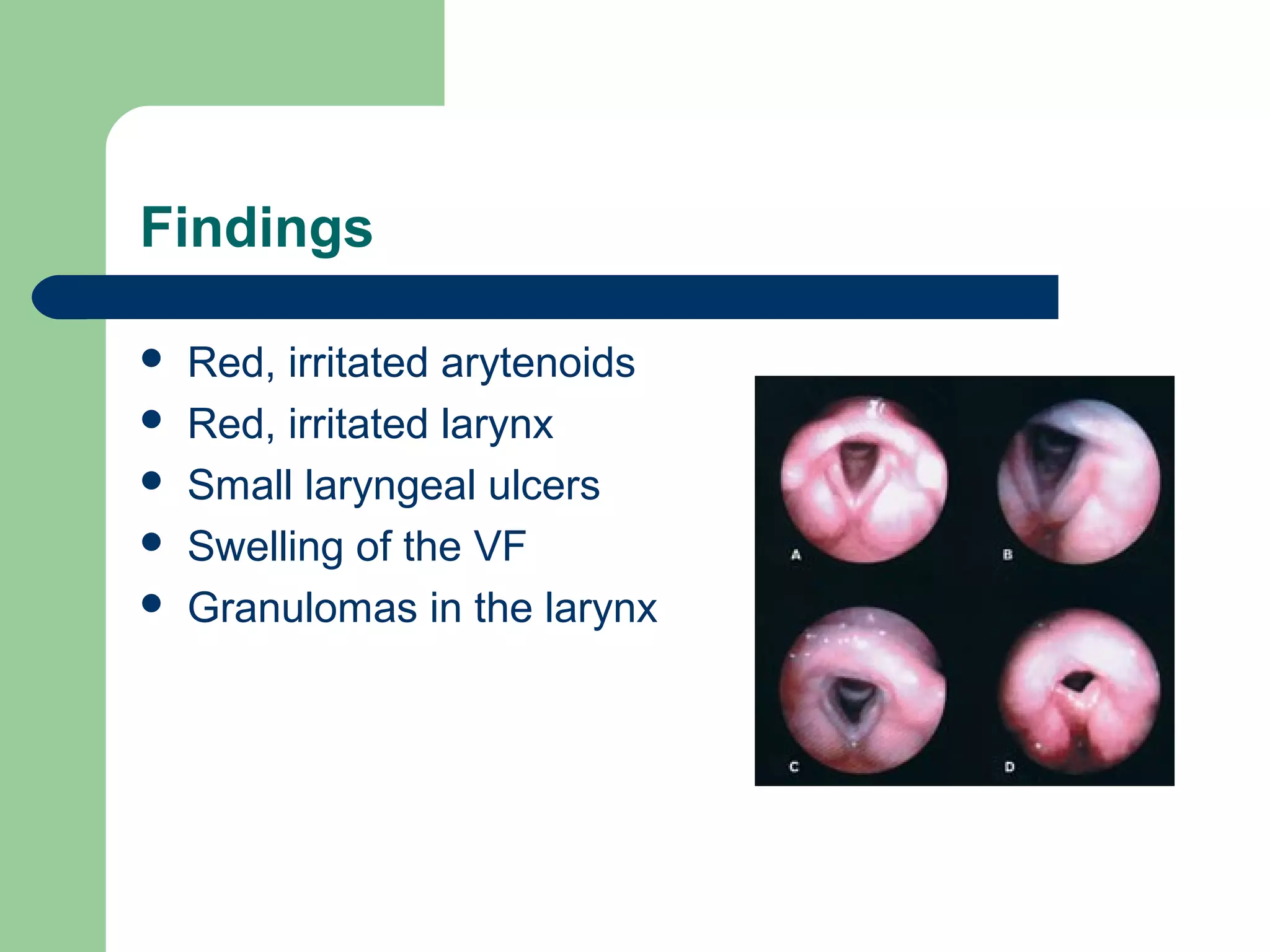
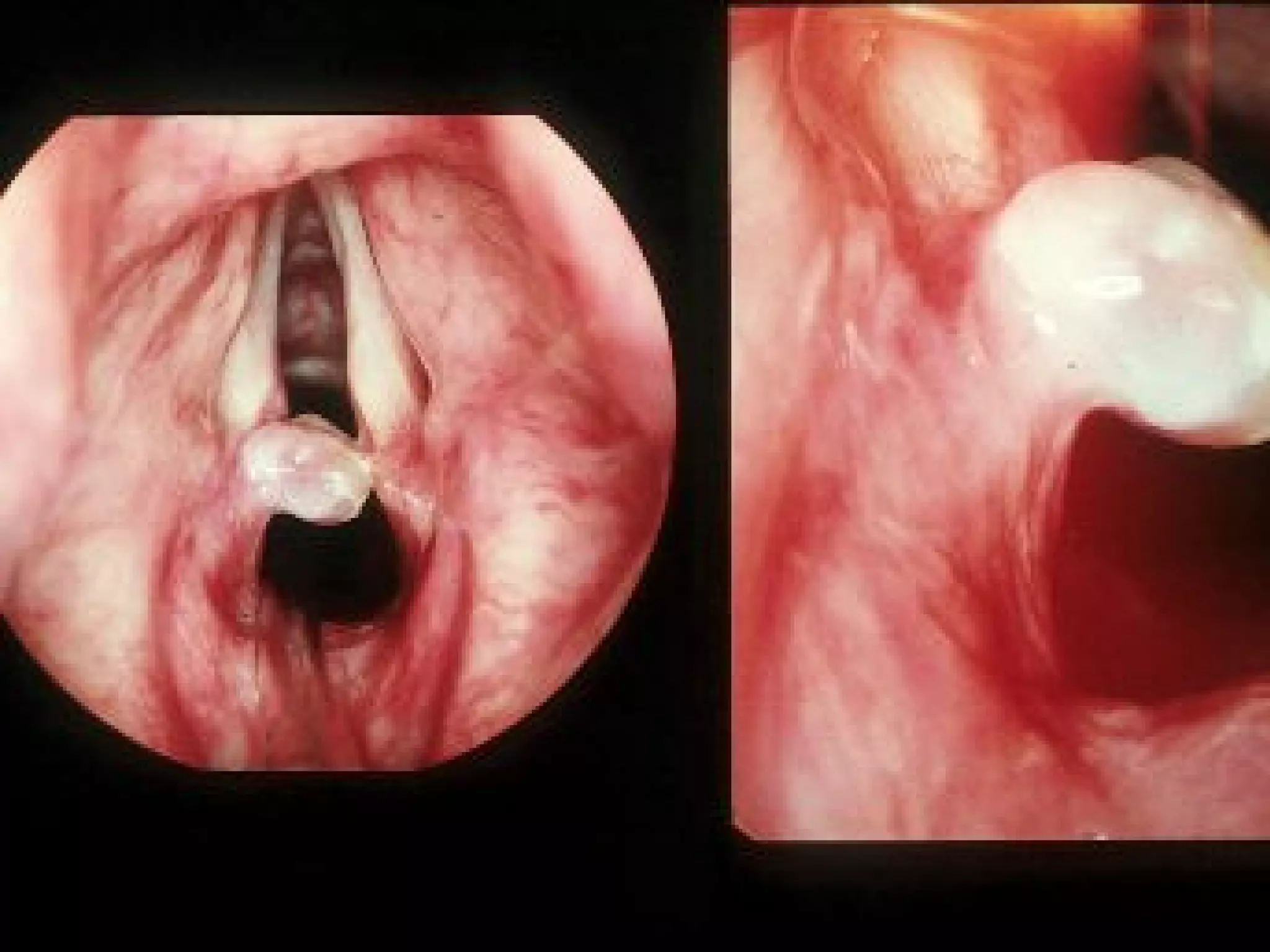
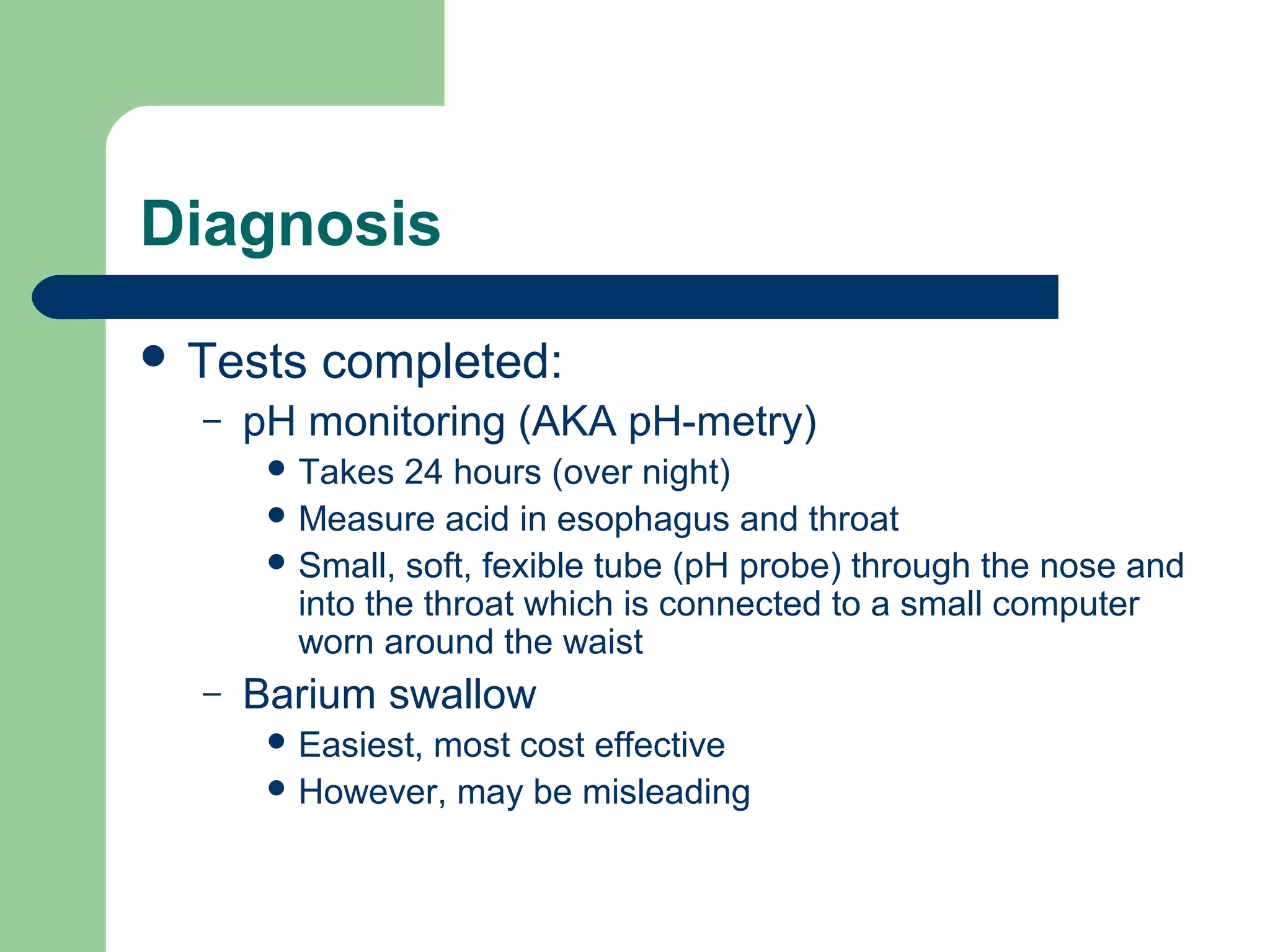
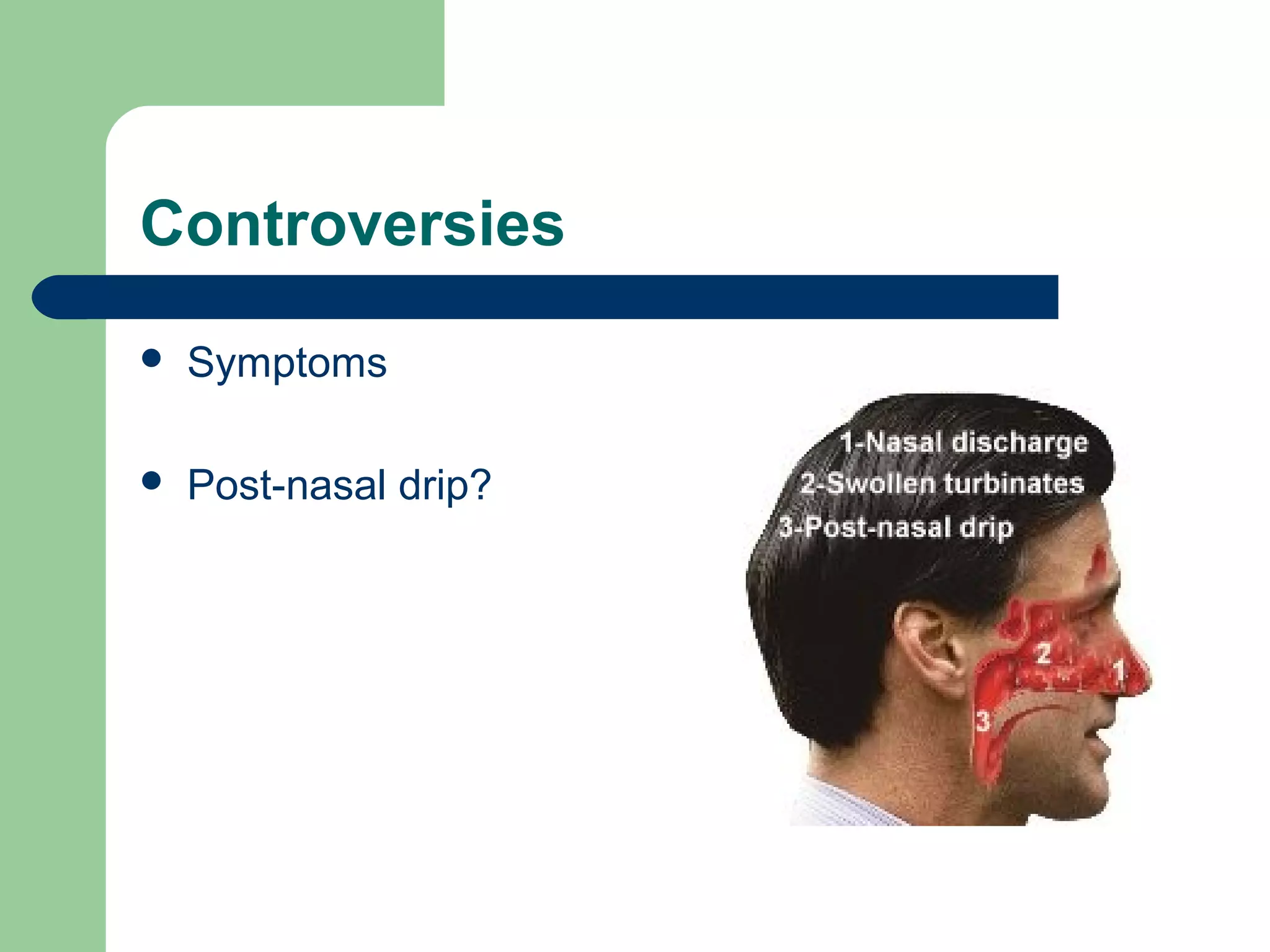
Gastroesophageal Reflux Disease (GERD) and Laryngopharyngeal Reflux Disease (LPRD) are conditions caused by backflow of stomach contents into the esophagus and throat. GERD causes heartburn and damage to the esophagus, while LPRD can cause throat clearing, cough, and voice problems from acid exposure to the larynx and throat. Diagnosis involves pH monitoring and treatment focuses on lifestyle changes, medications, and sometimes surgery to tighten the lower esophageal sphincter and reduce reflux. Controversies exist regarding diagnostic testing and treatment approaches for LPRD.