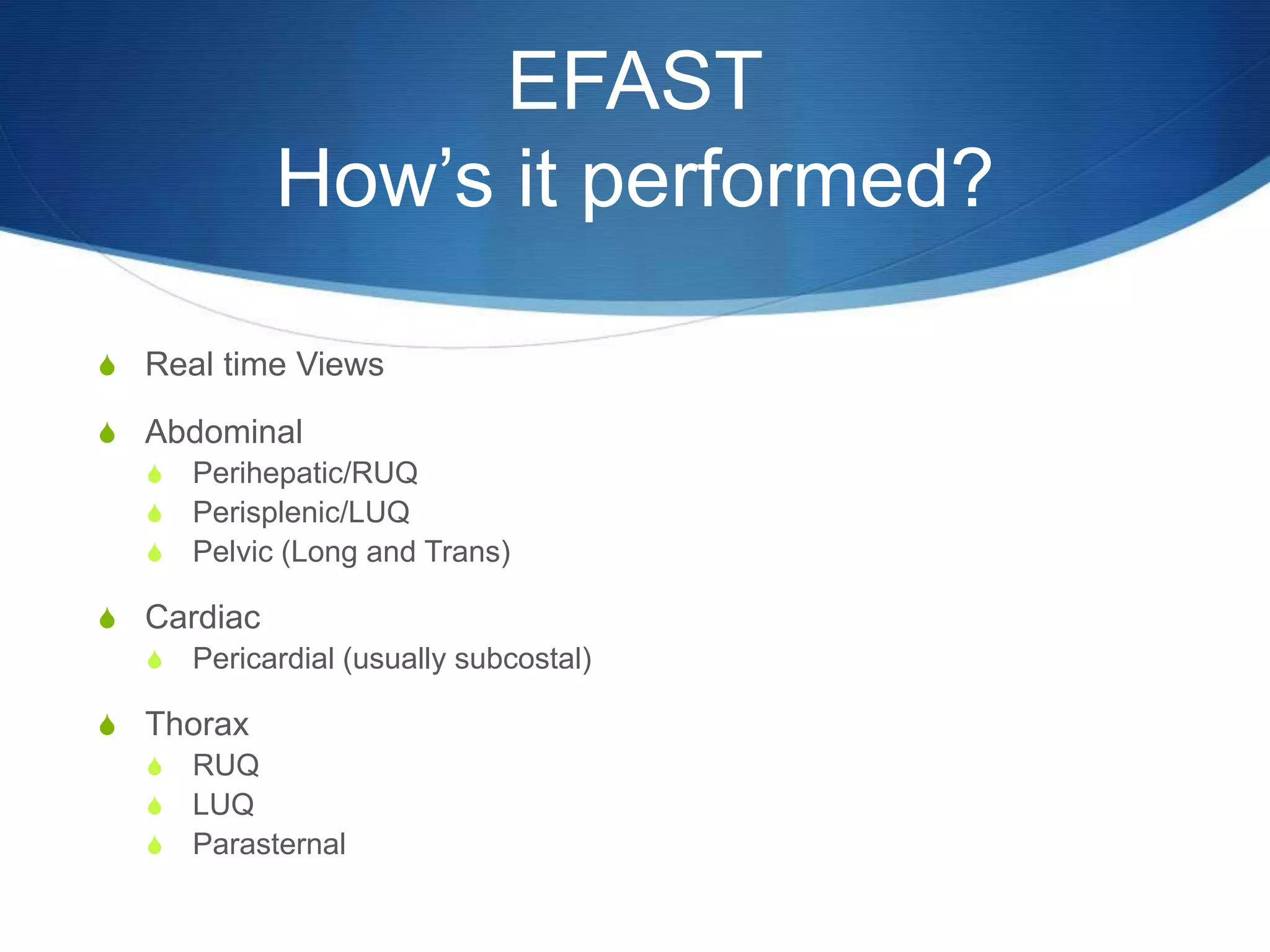
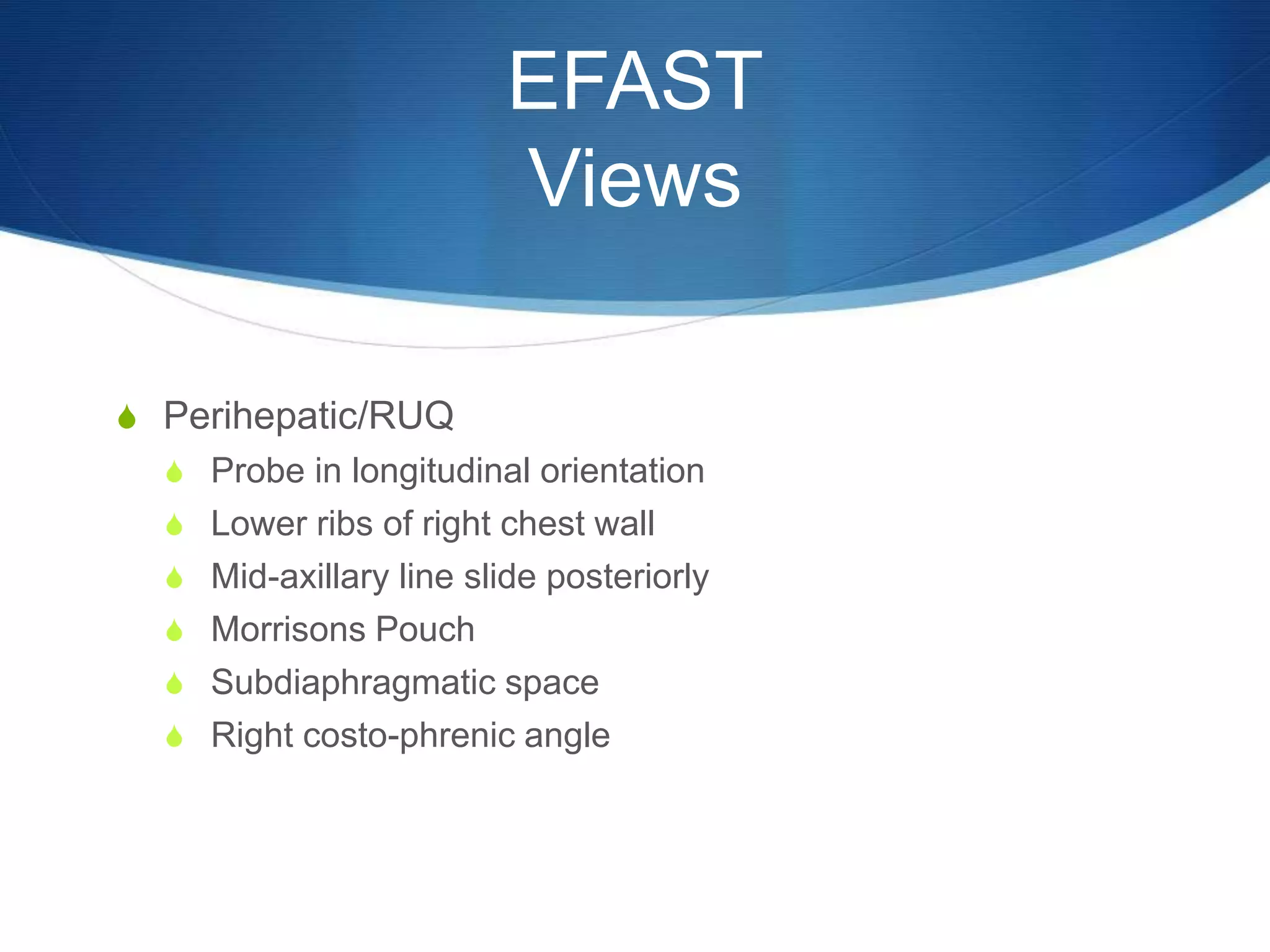
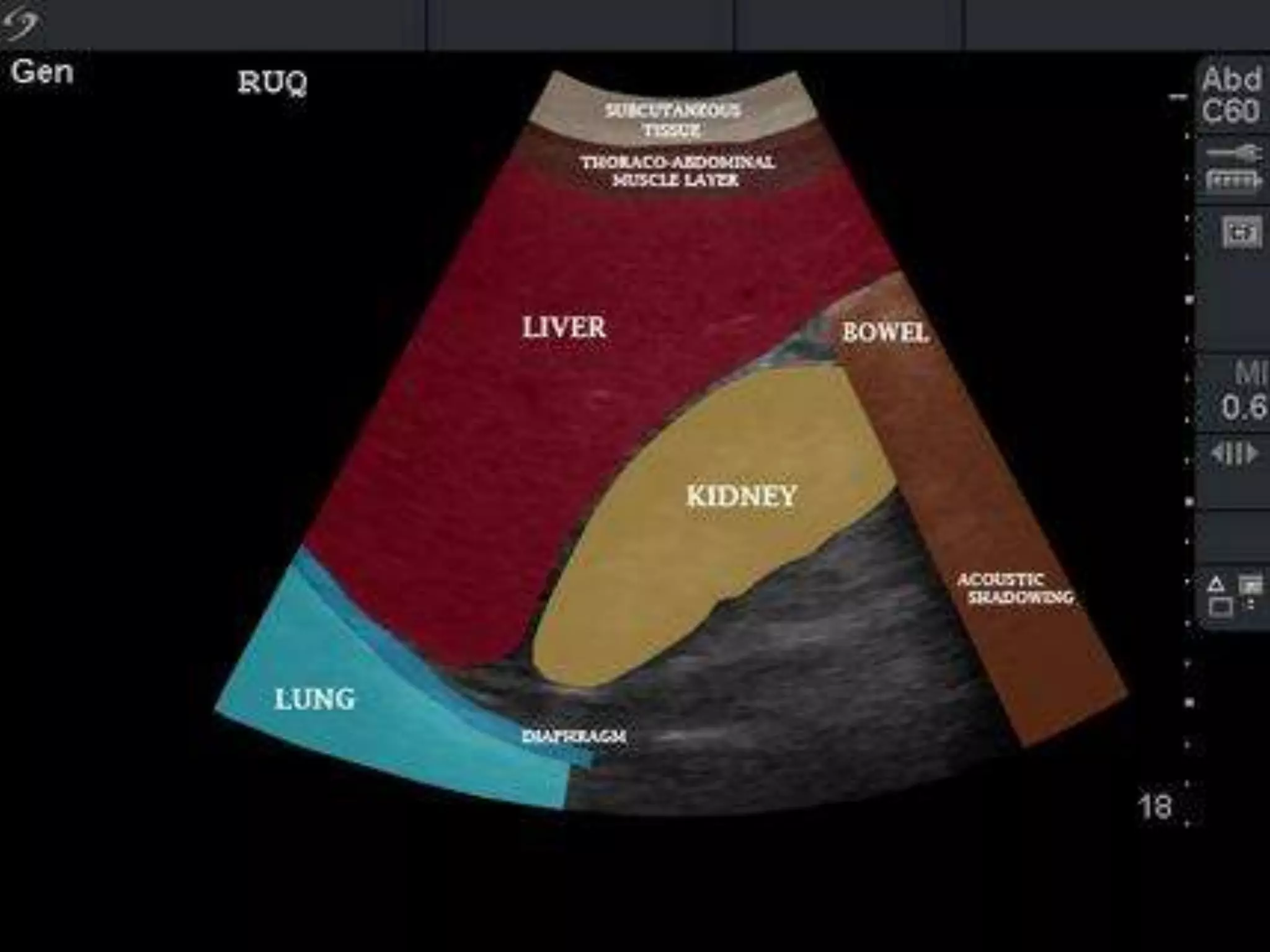
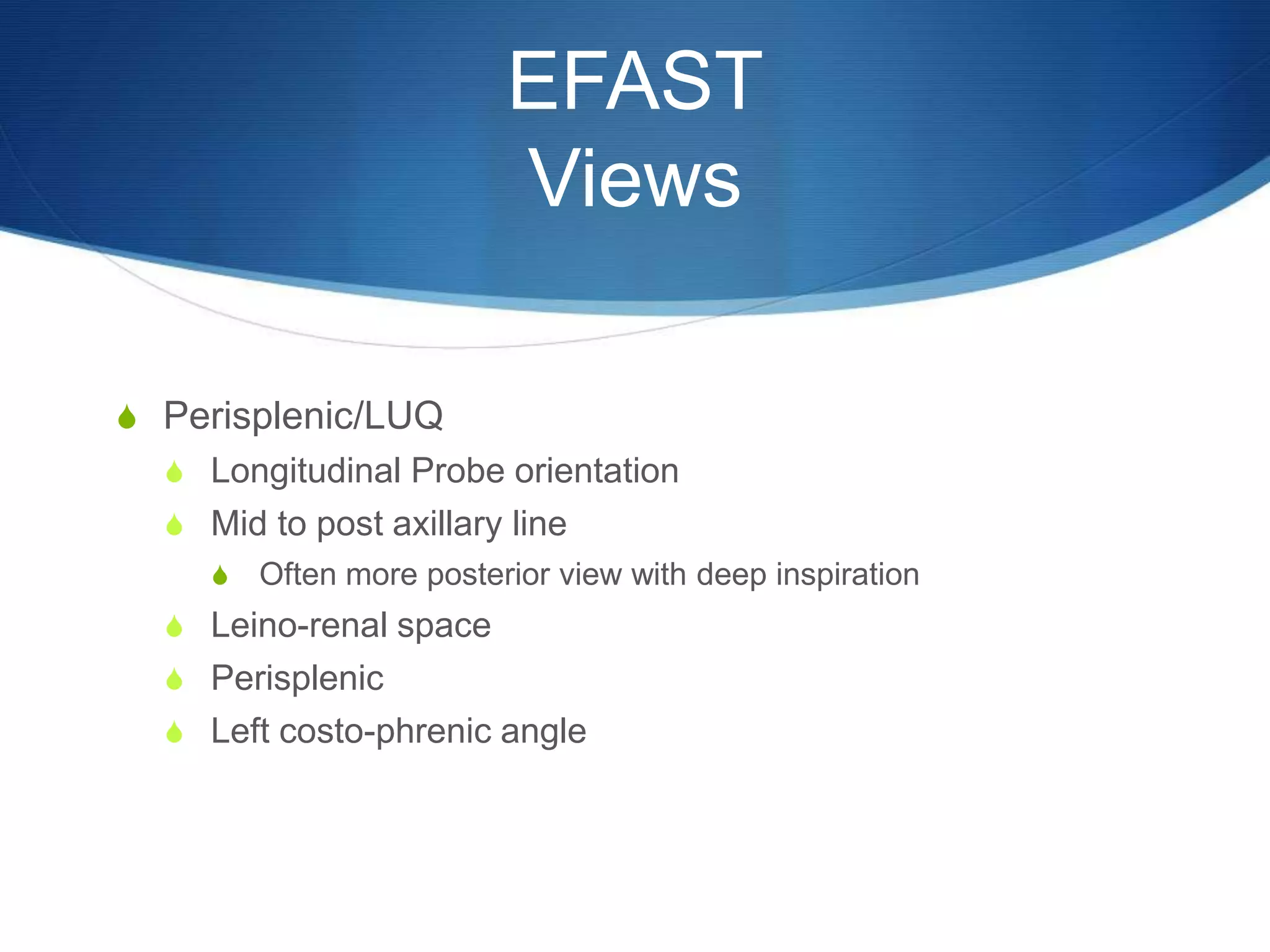
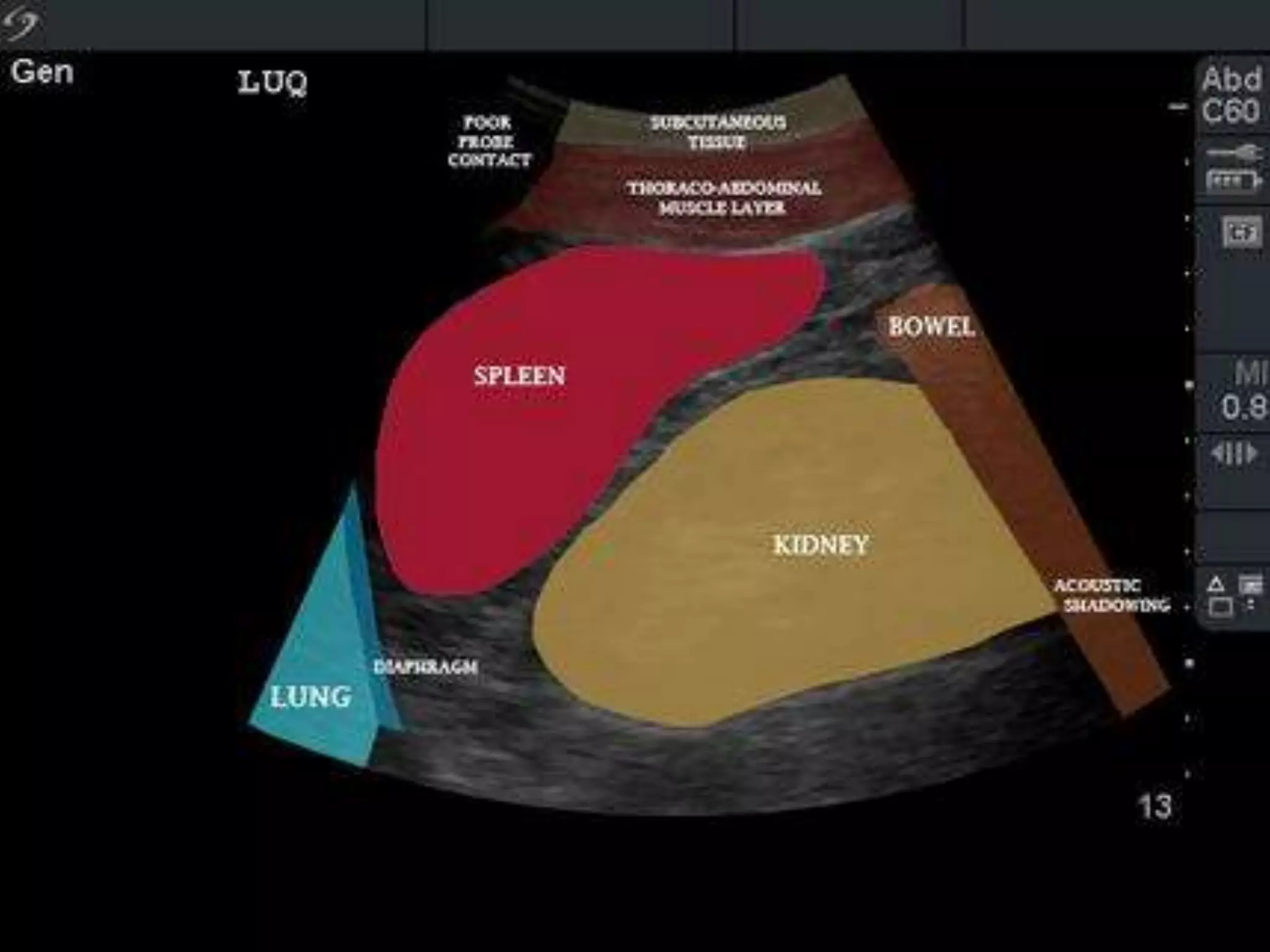
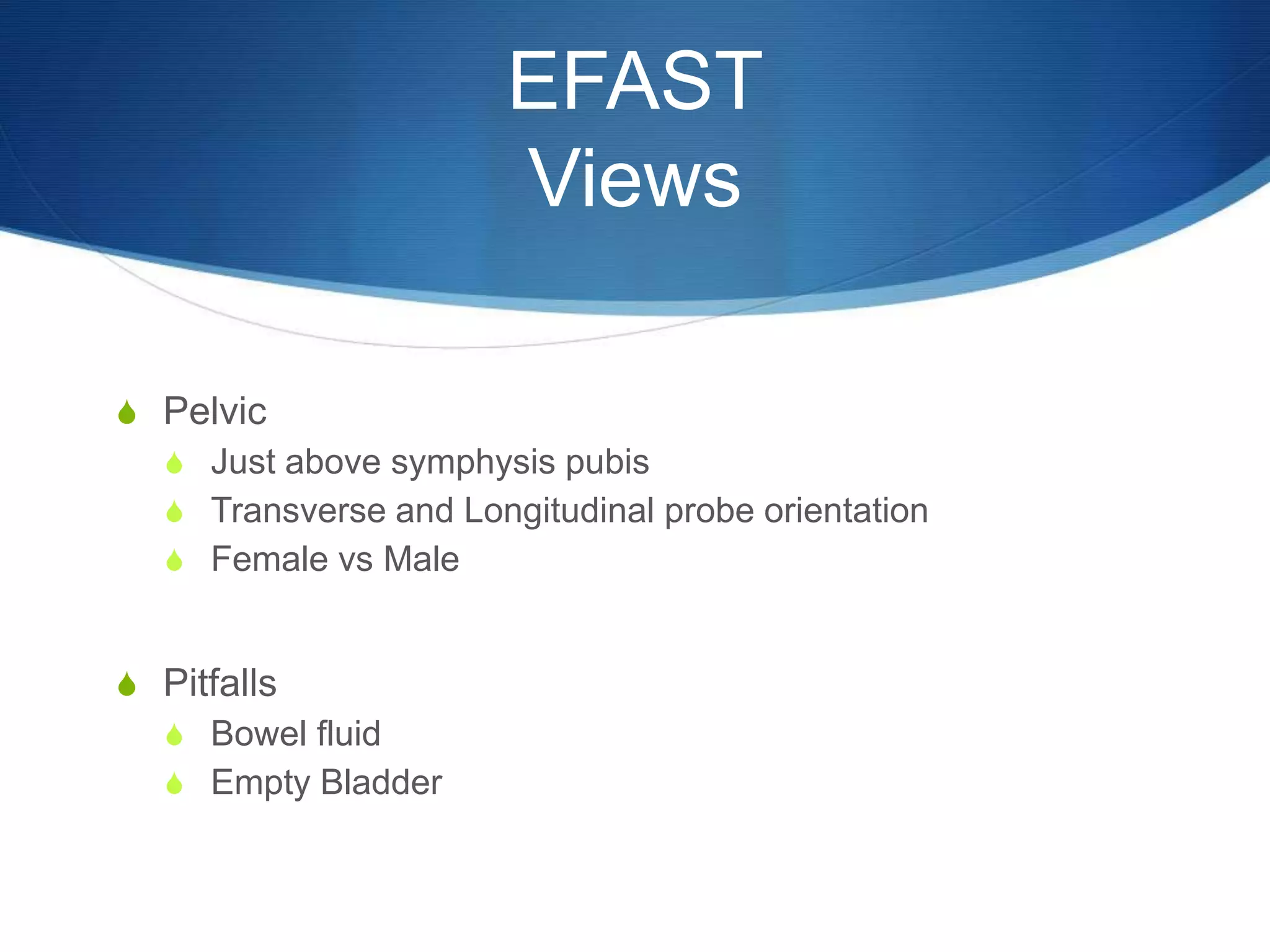
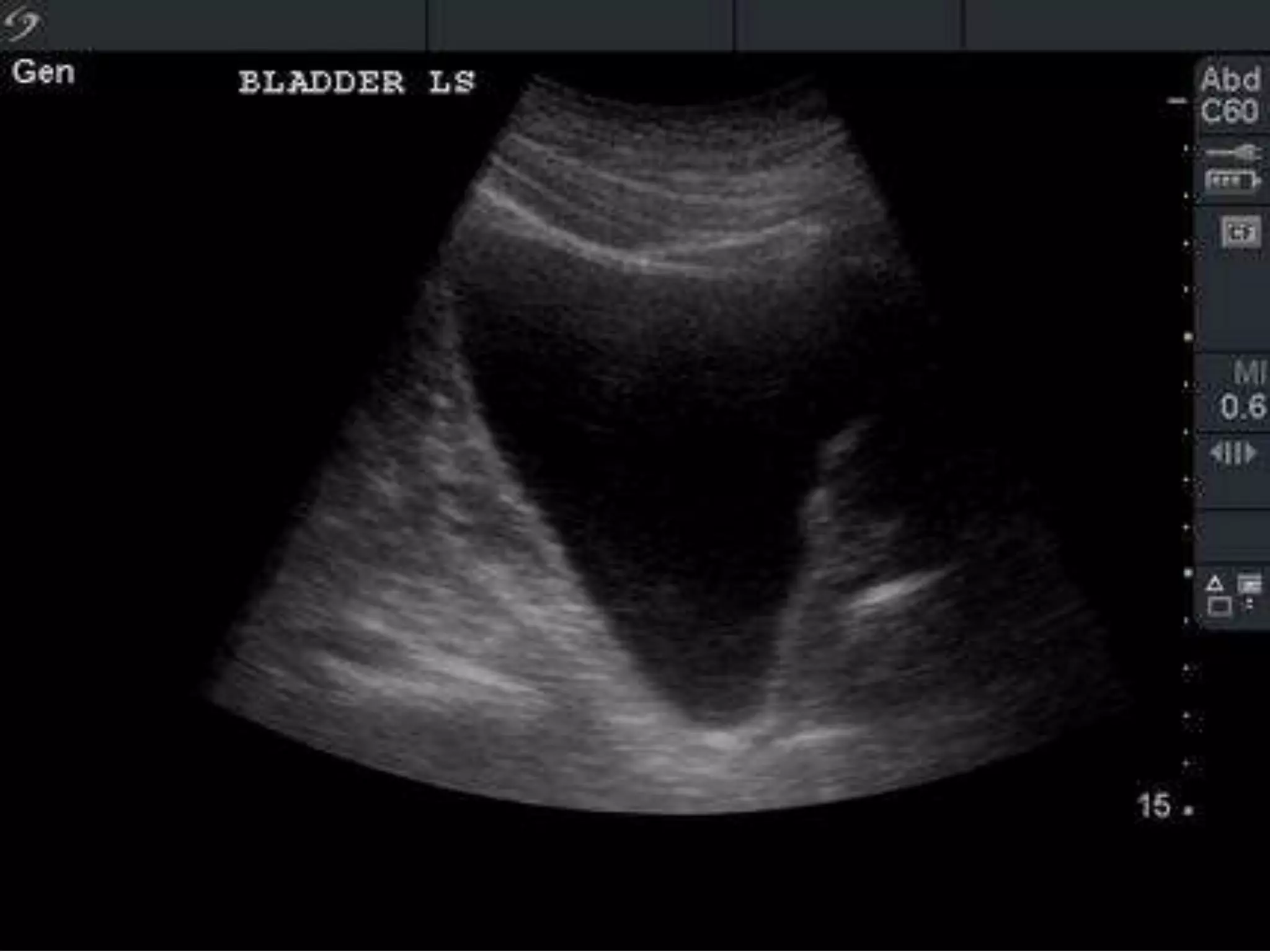
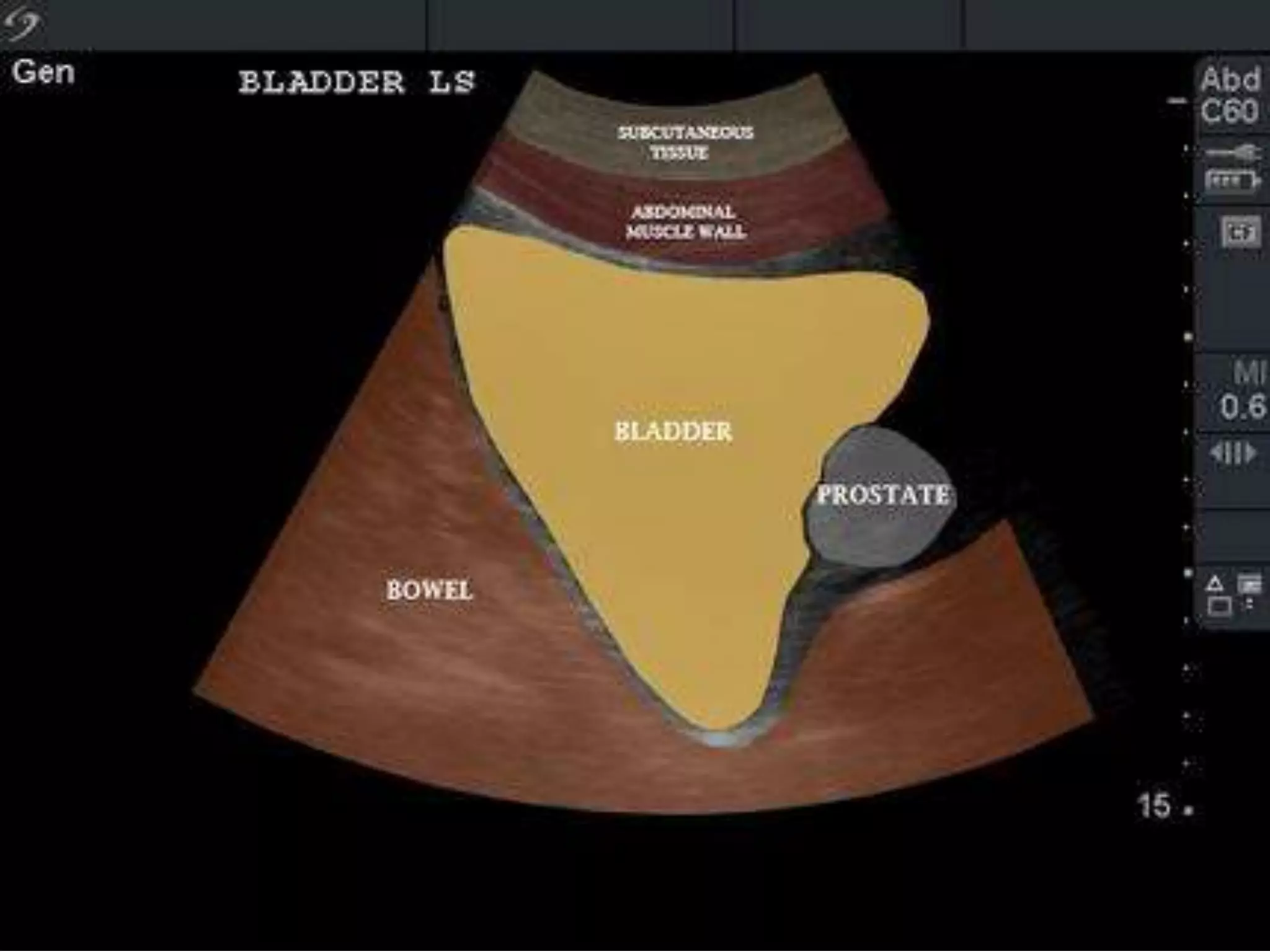
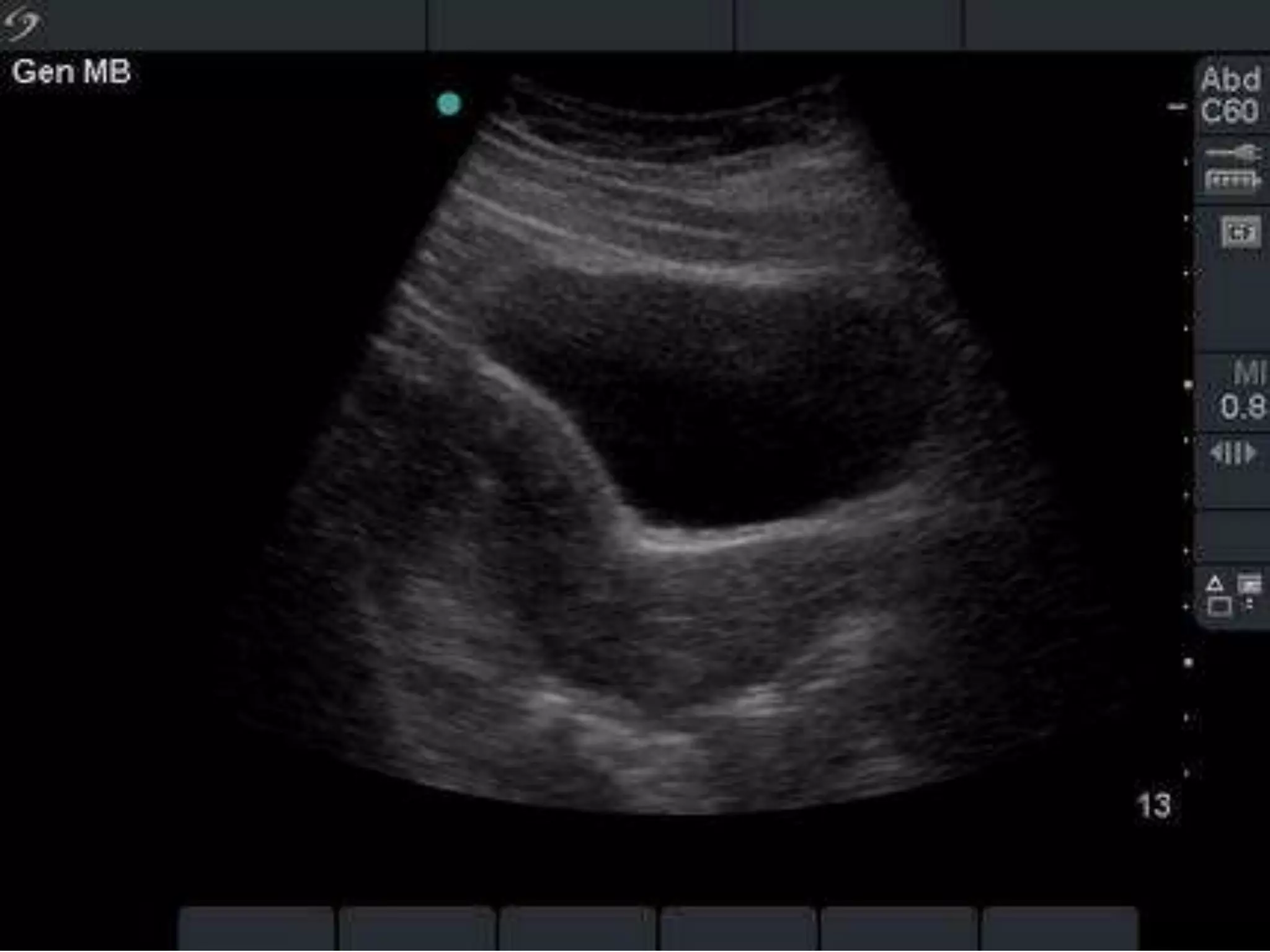
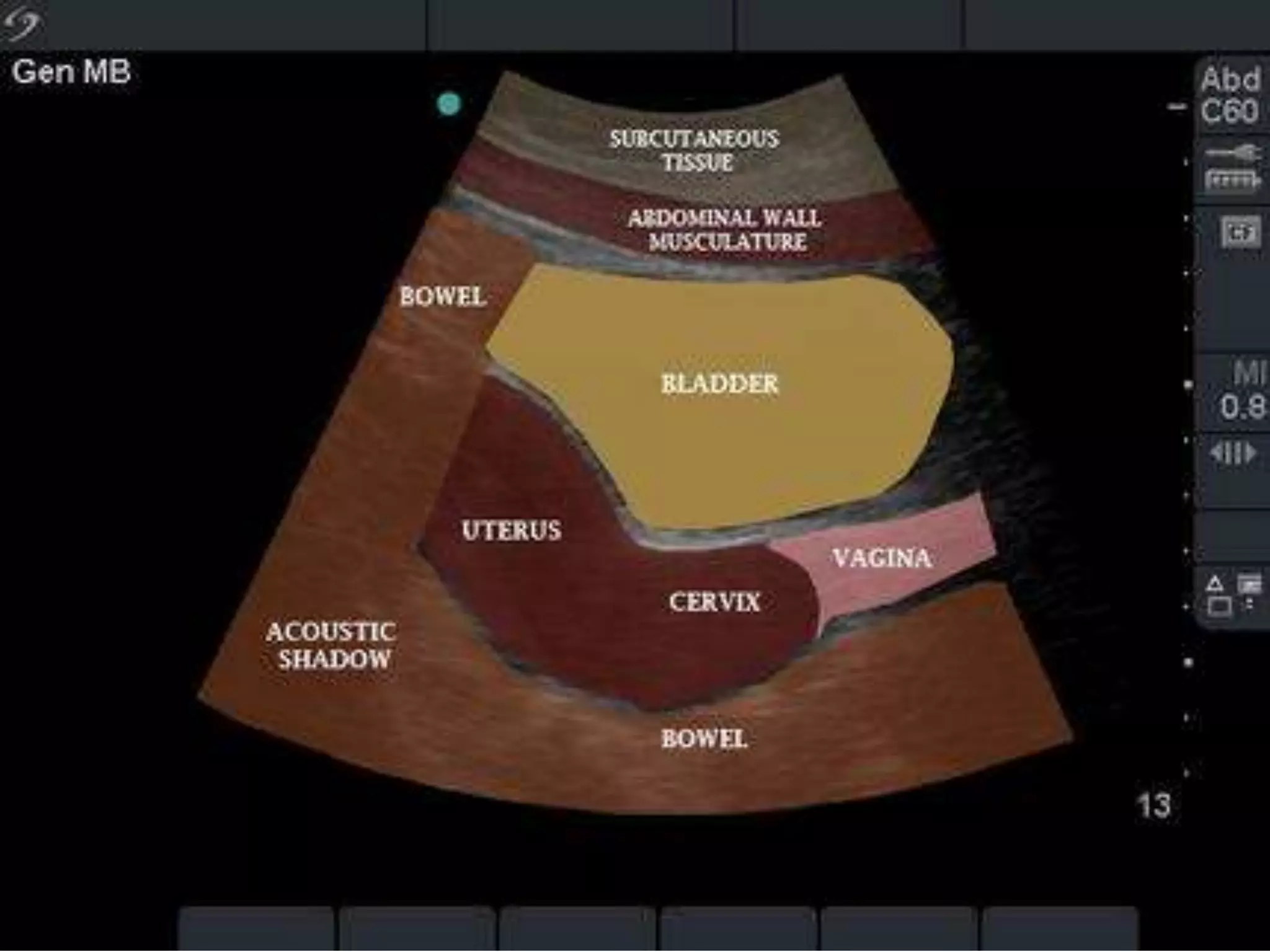
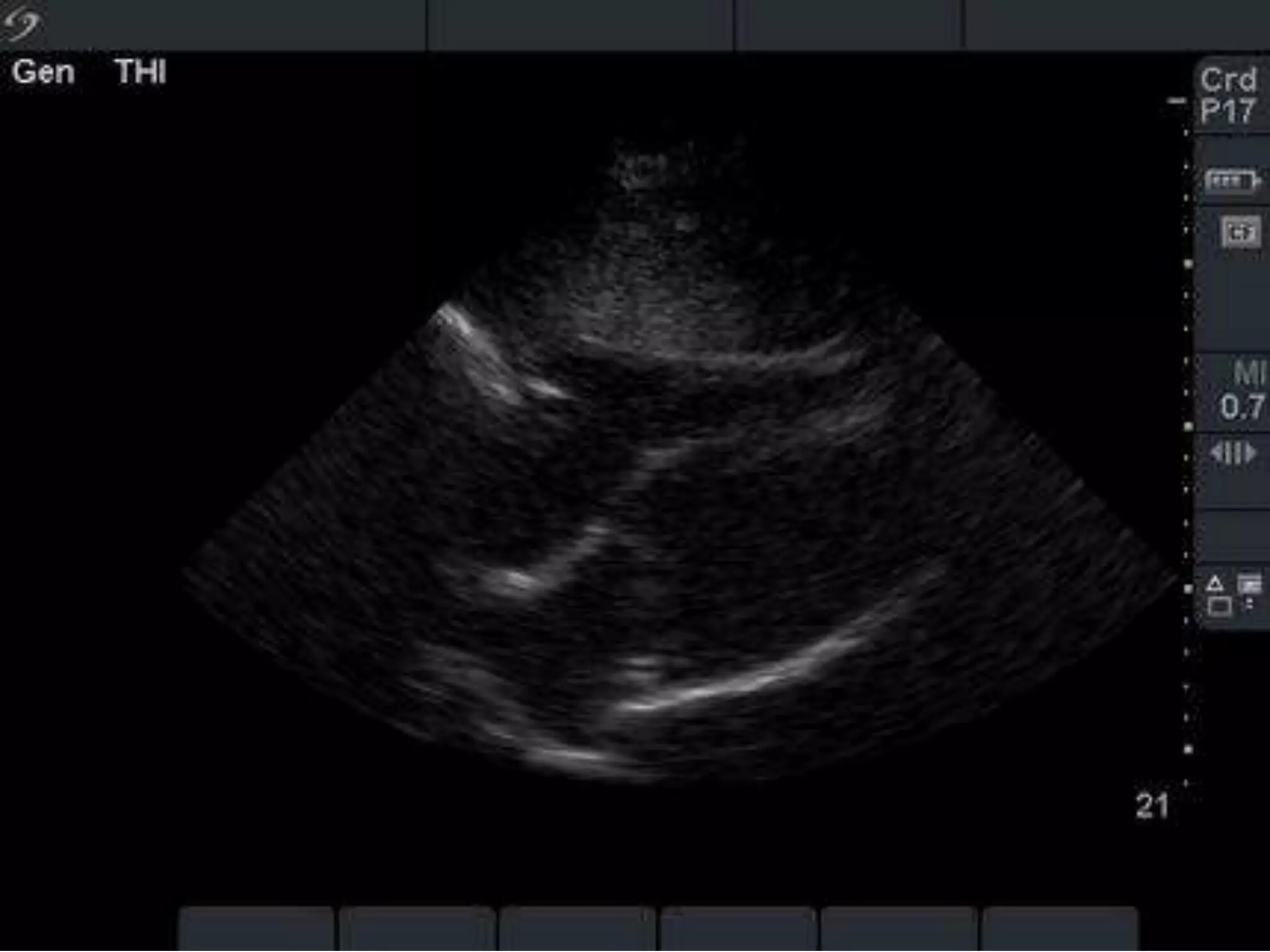
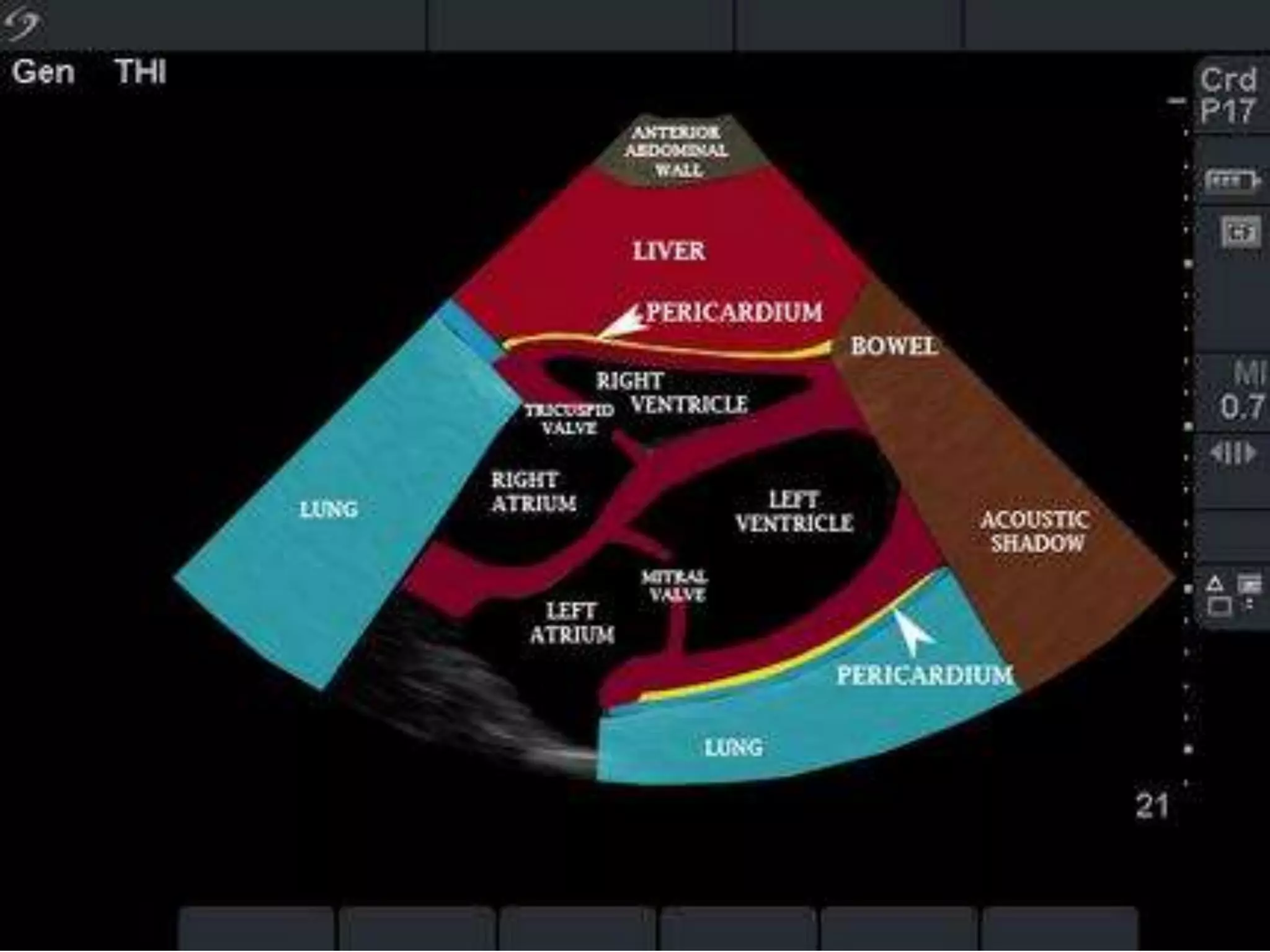
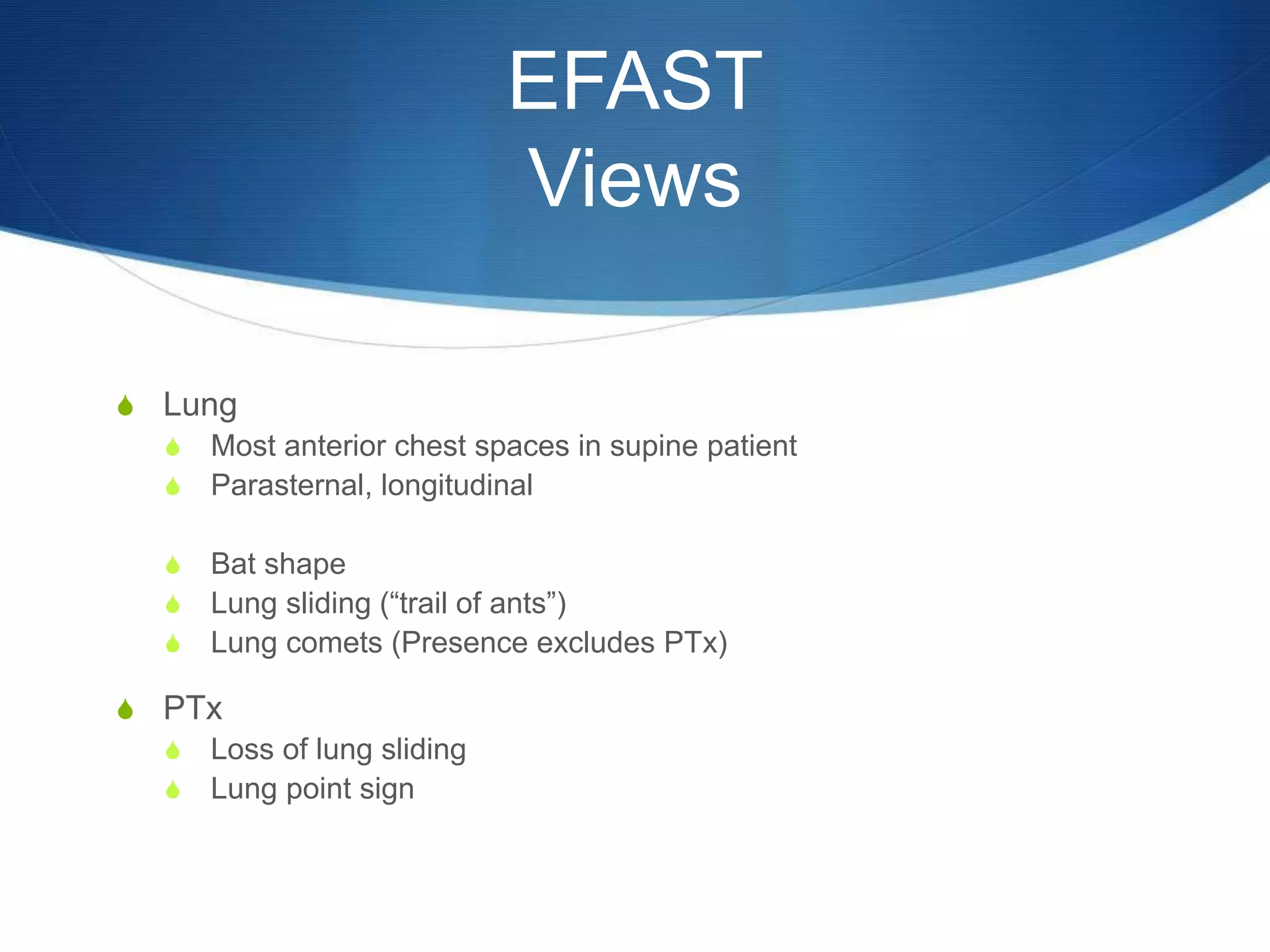
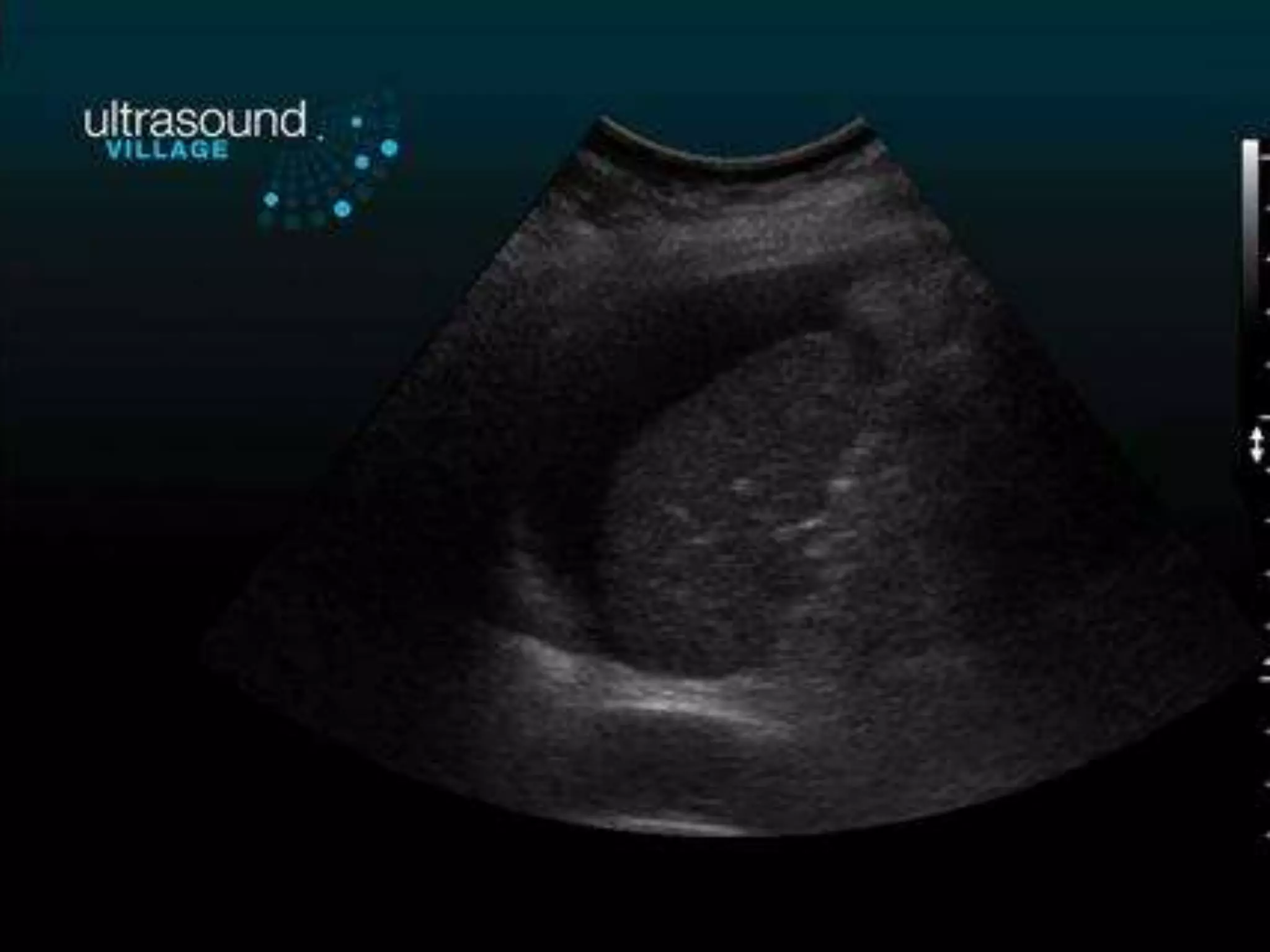
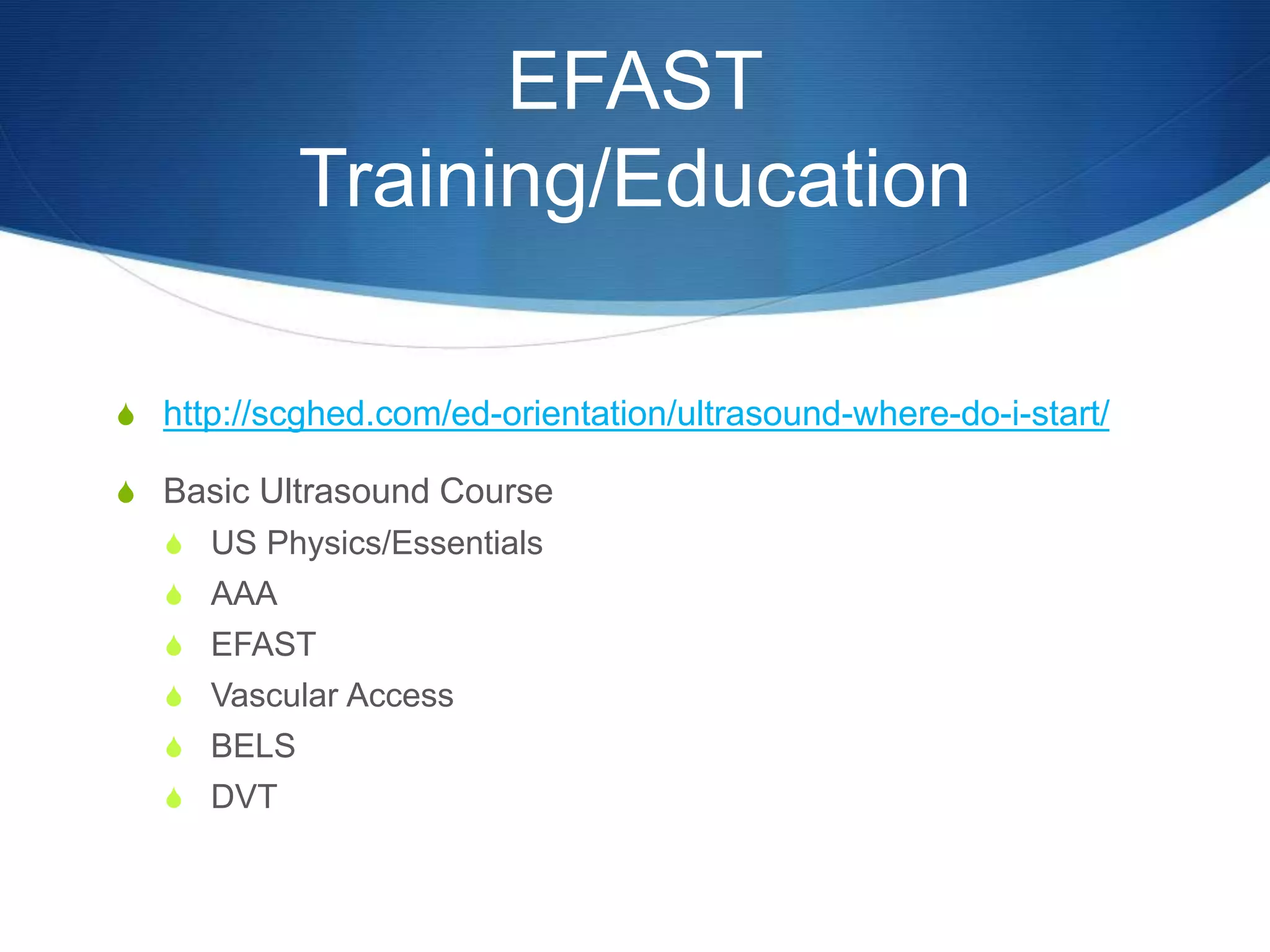
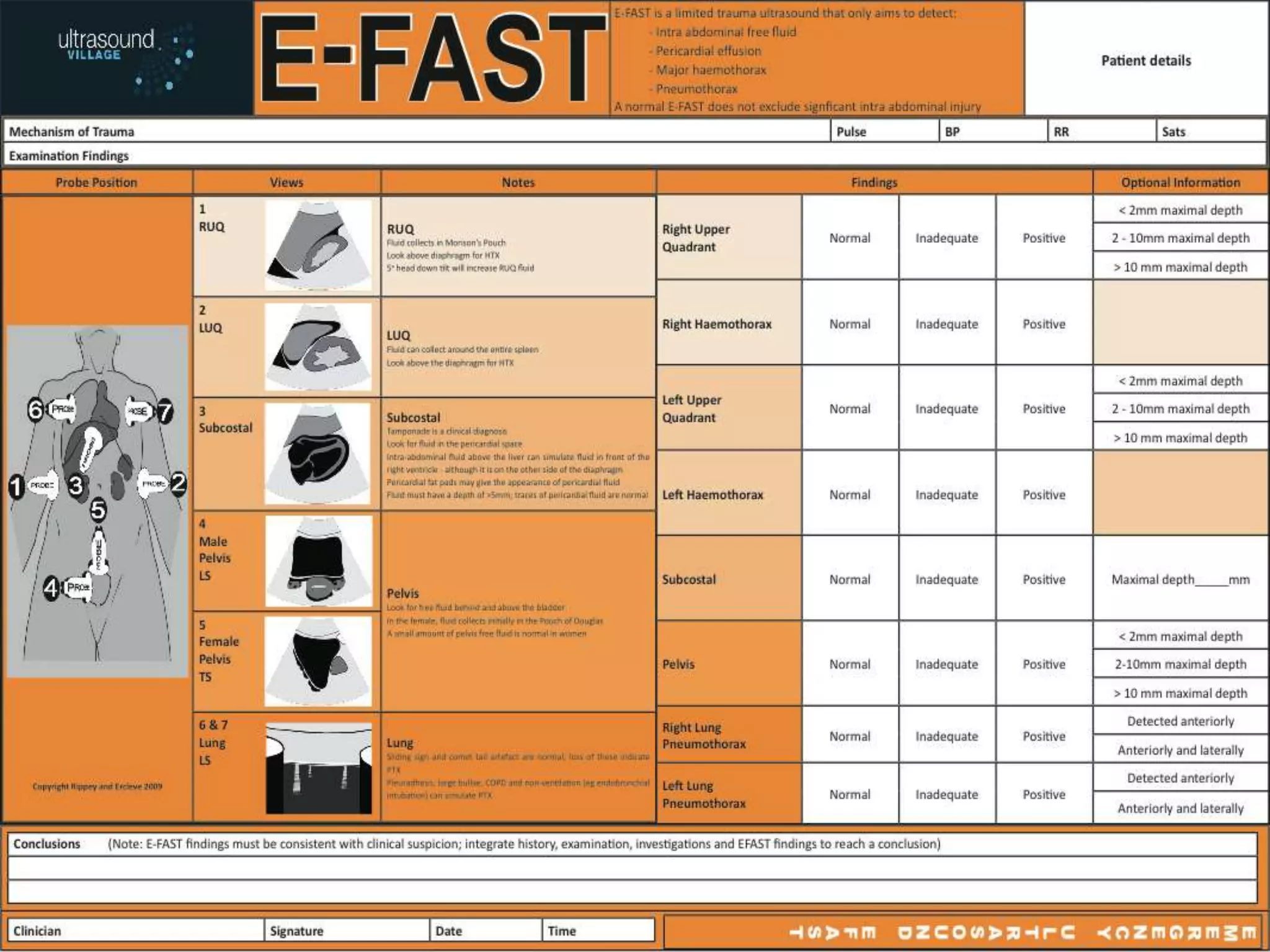
This document provides an overview of the EFAST (Extended Focused Assessment with Sonography in Trauma) scan. It describes the objectives, definition, views, and techniques used in an EFAST exam to rapidly assess trauma patients for free fluid in the abdomen, chest, or pericardium. The advantages of EFAST are discussed, such as its speed, non-invasiveness, and ability to guide trauma management. Limitations include operator dependence and inability to differentiate fluid types. Training requirements are also outlined.