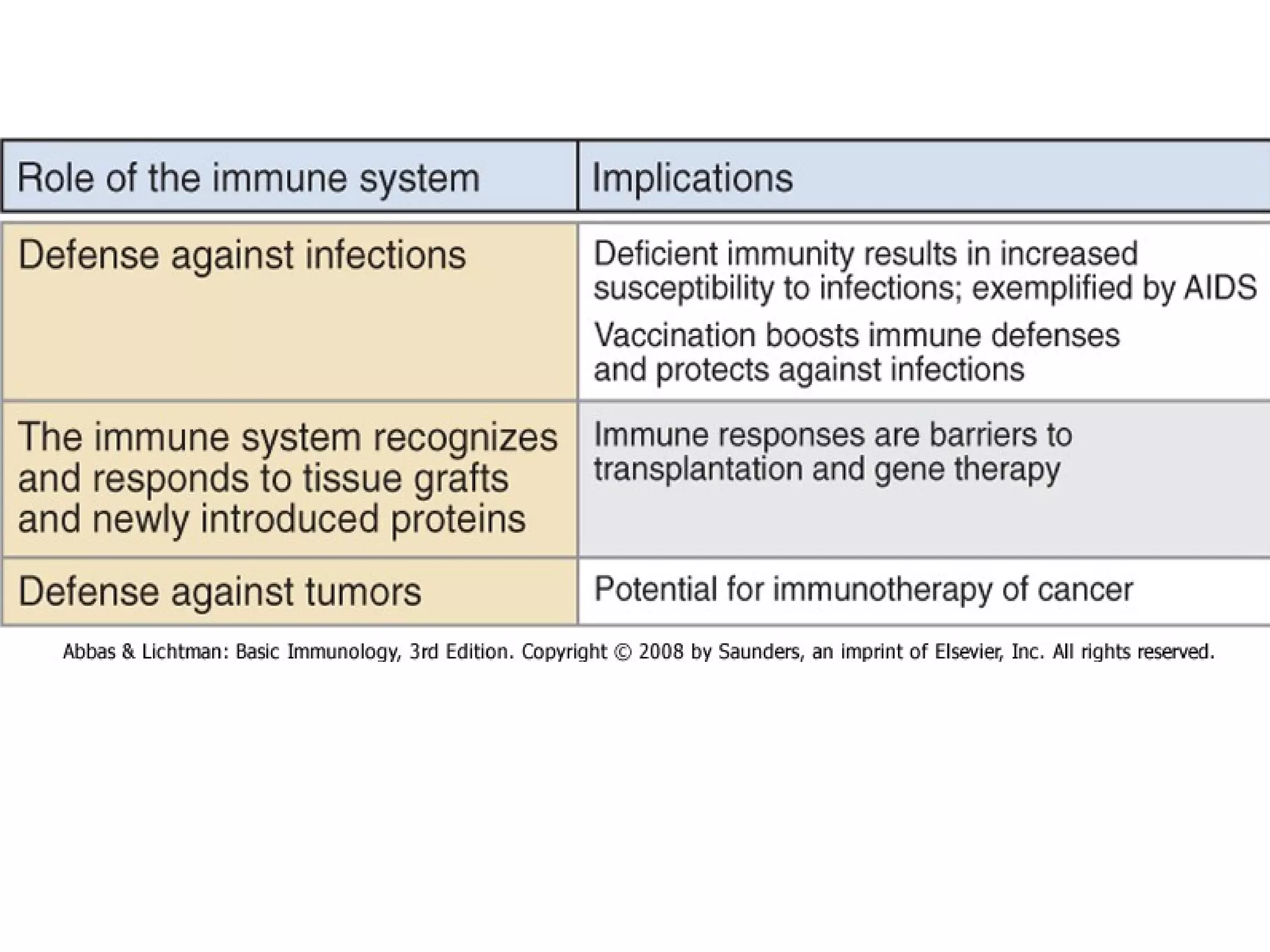
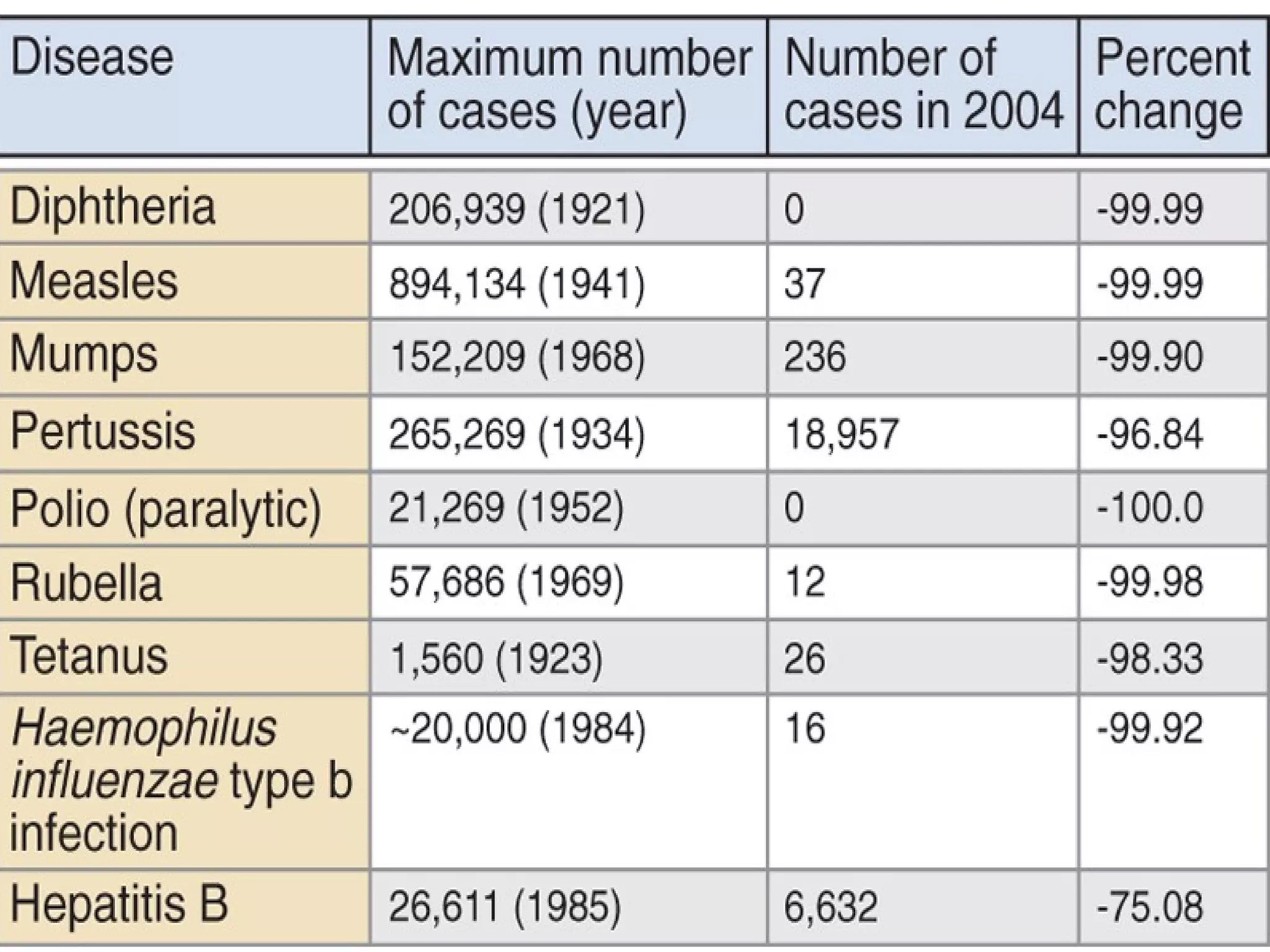
The document provides an overview of the immune system, including:
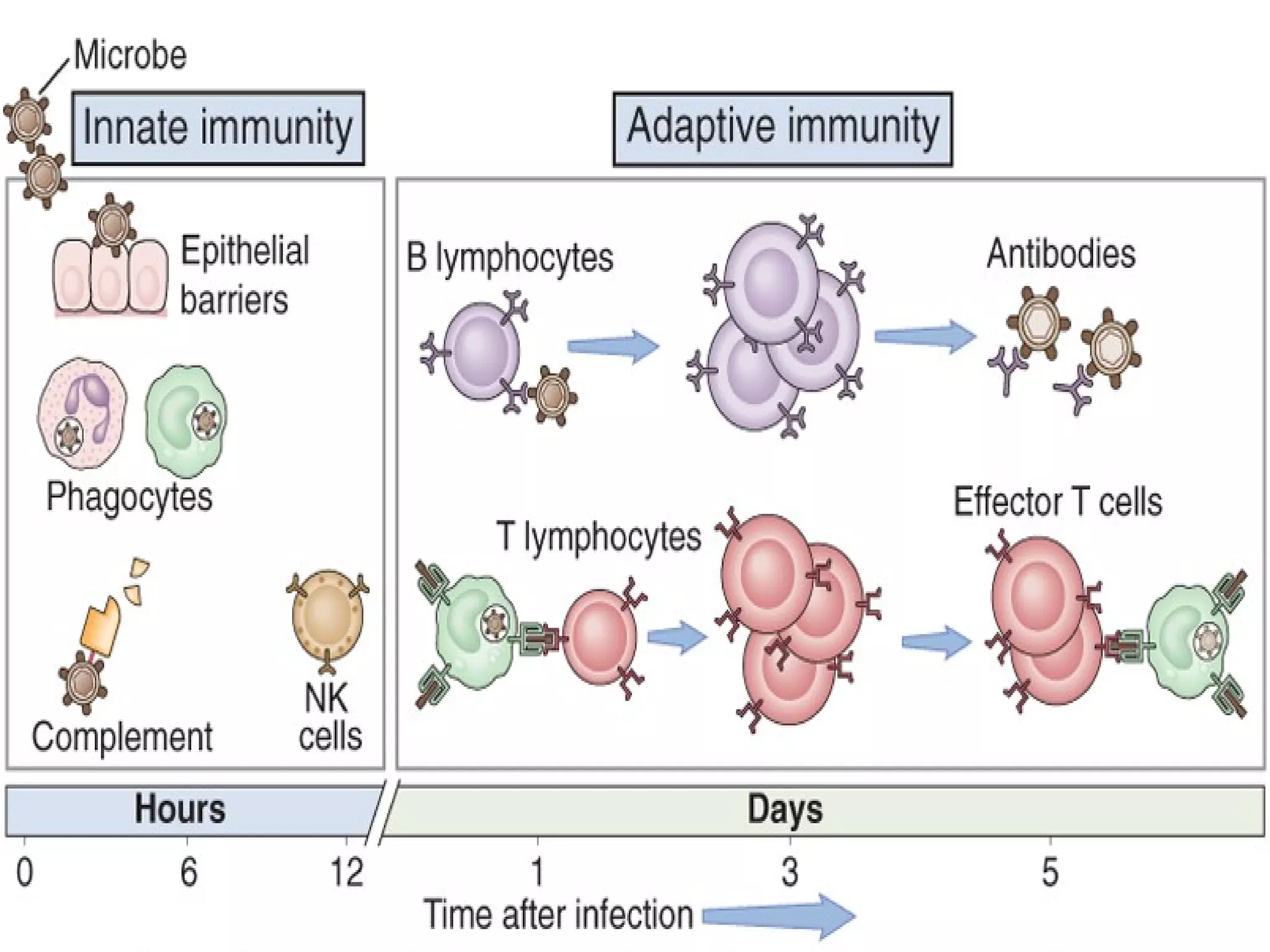
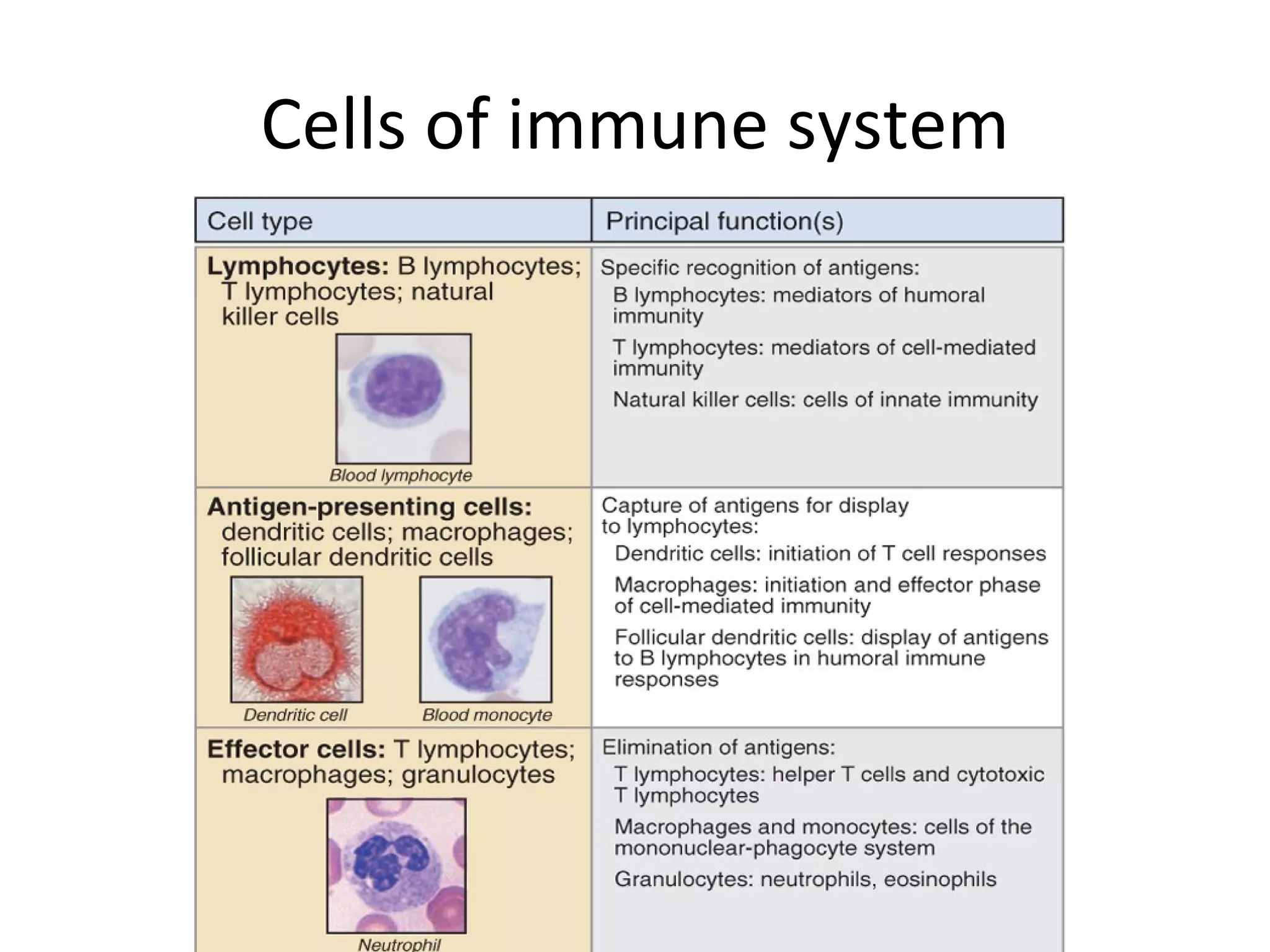
- Innate immunity acts as the first line of defense through barriers like skin and mucous membranes. Adaptive immunity responds later with targeted responses.
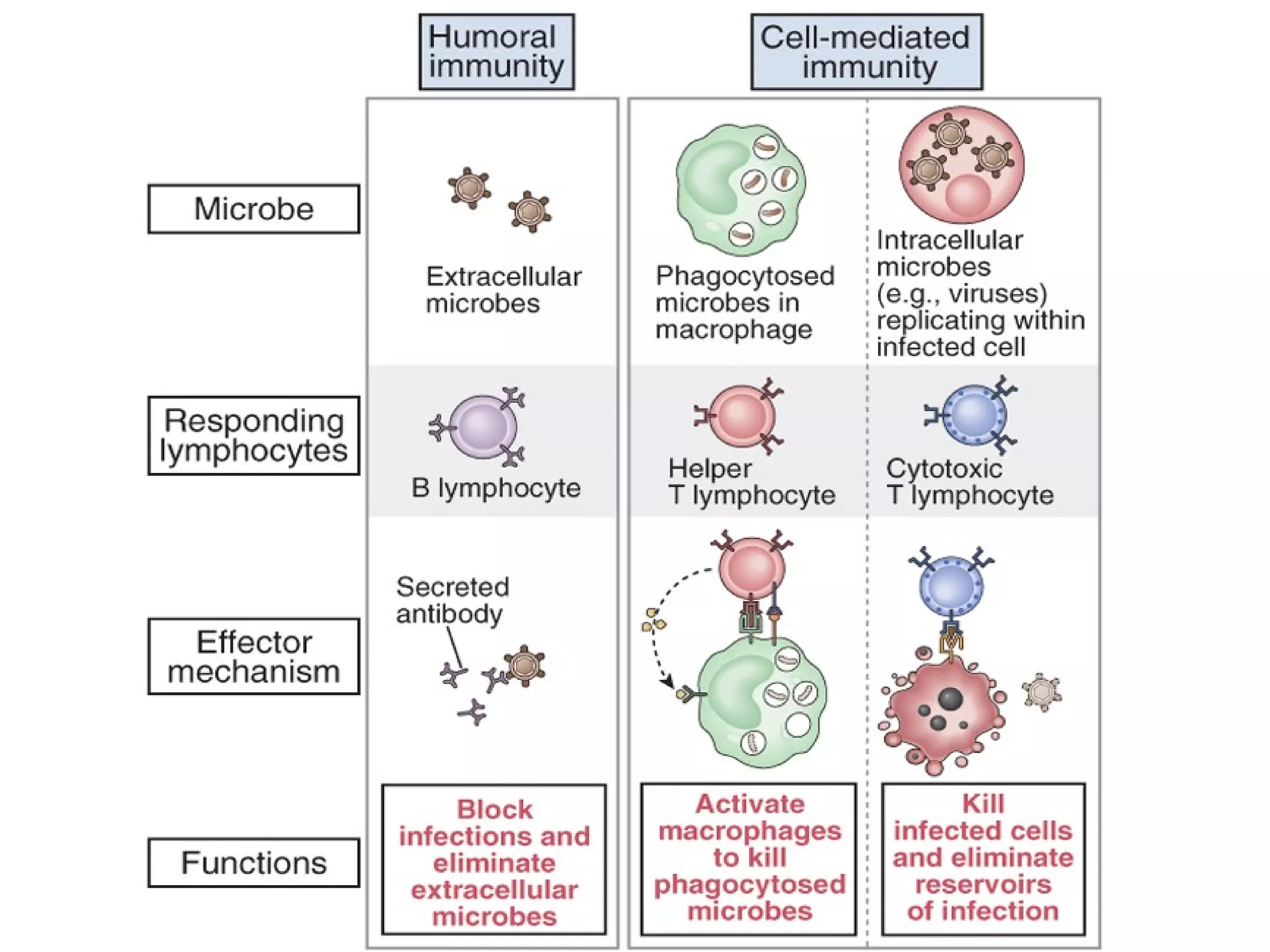
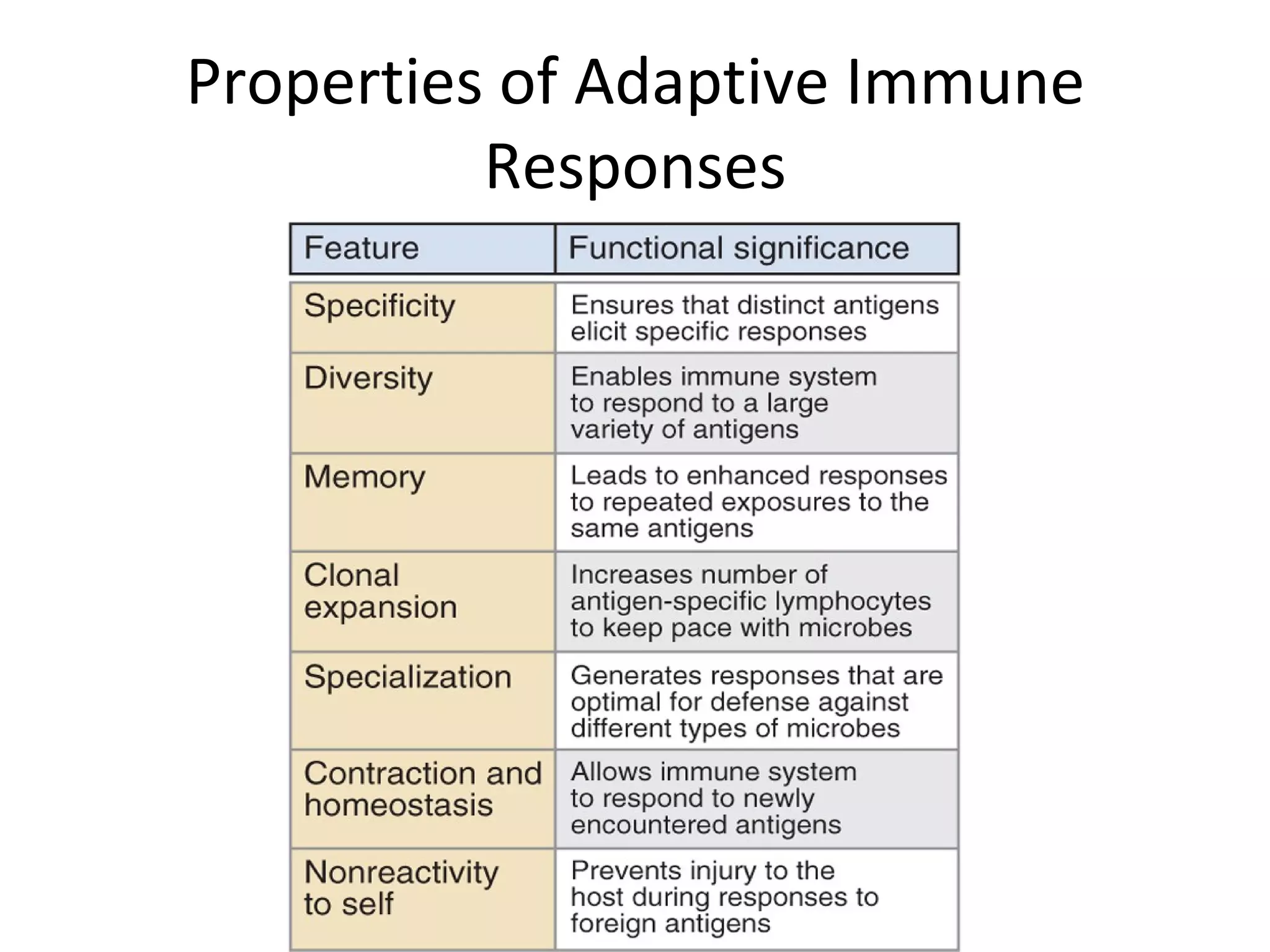
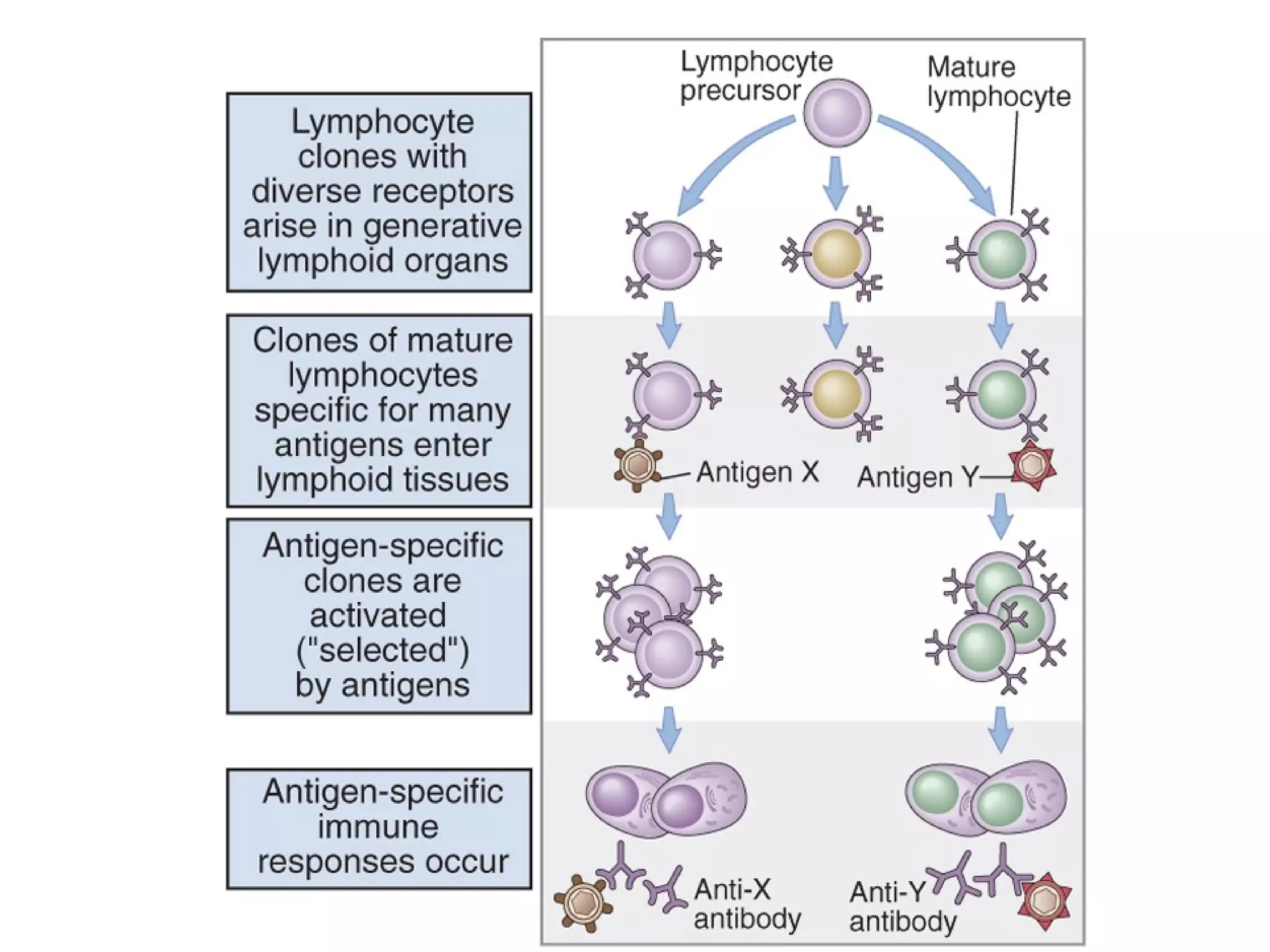
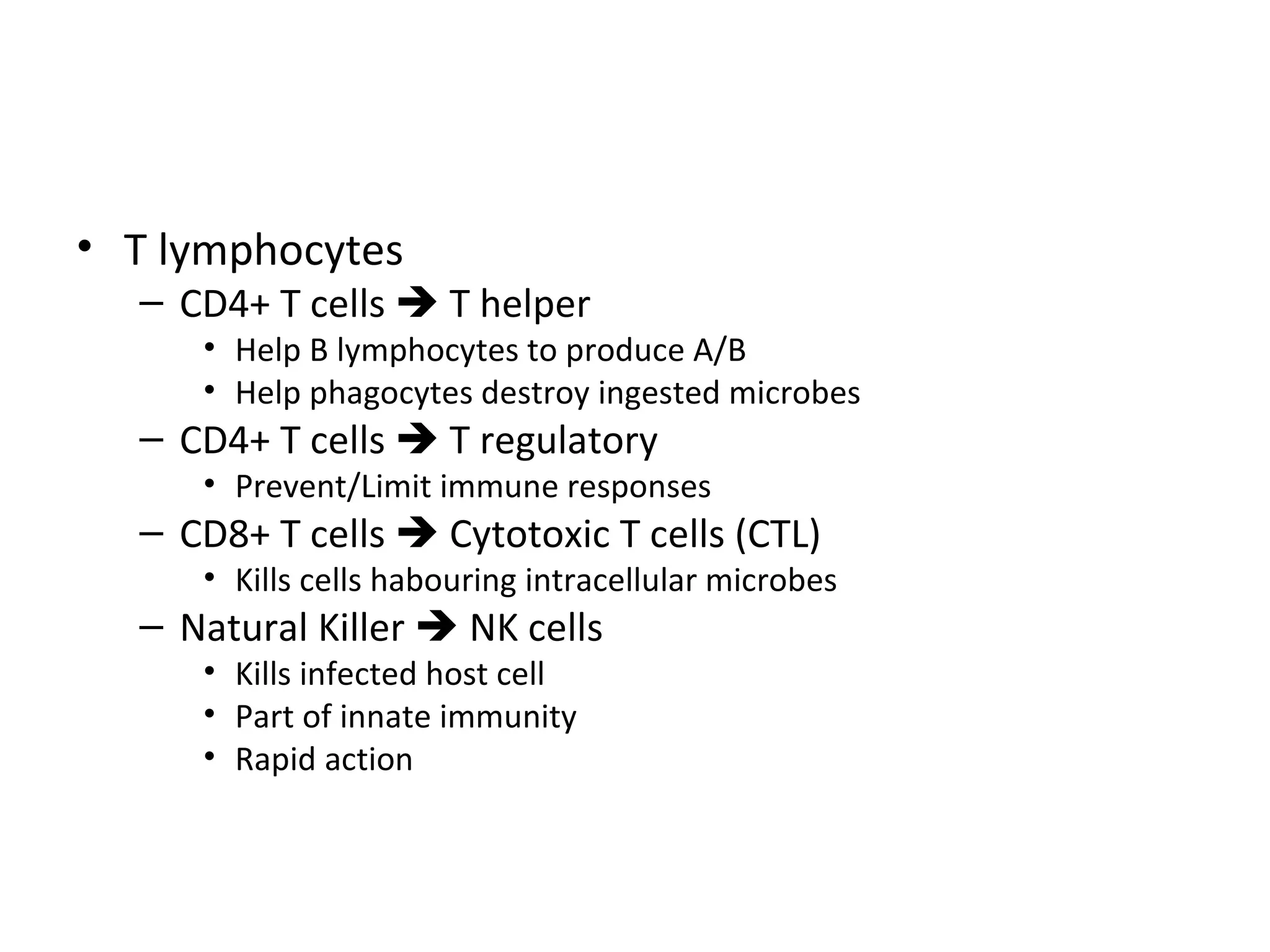
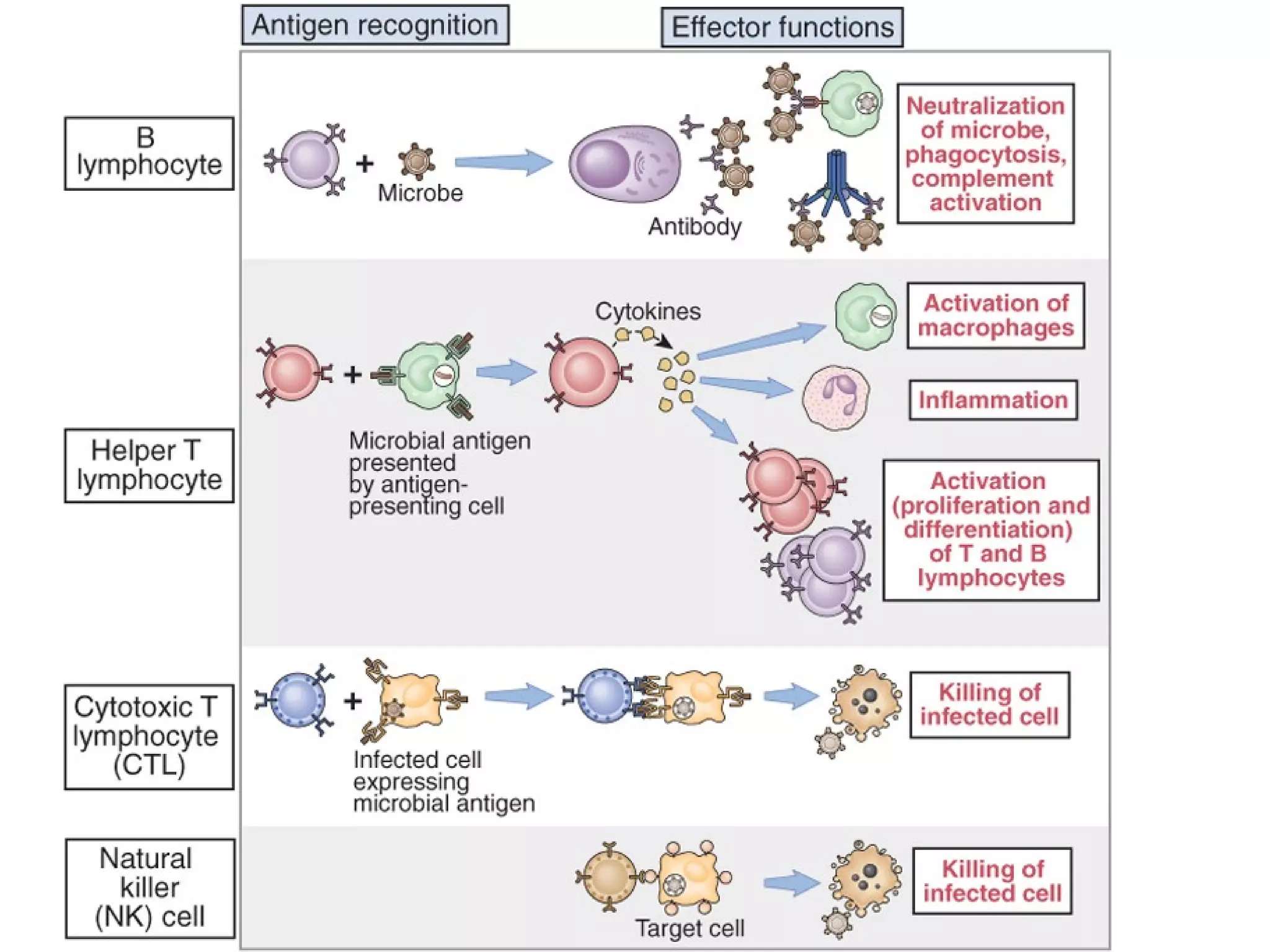
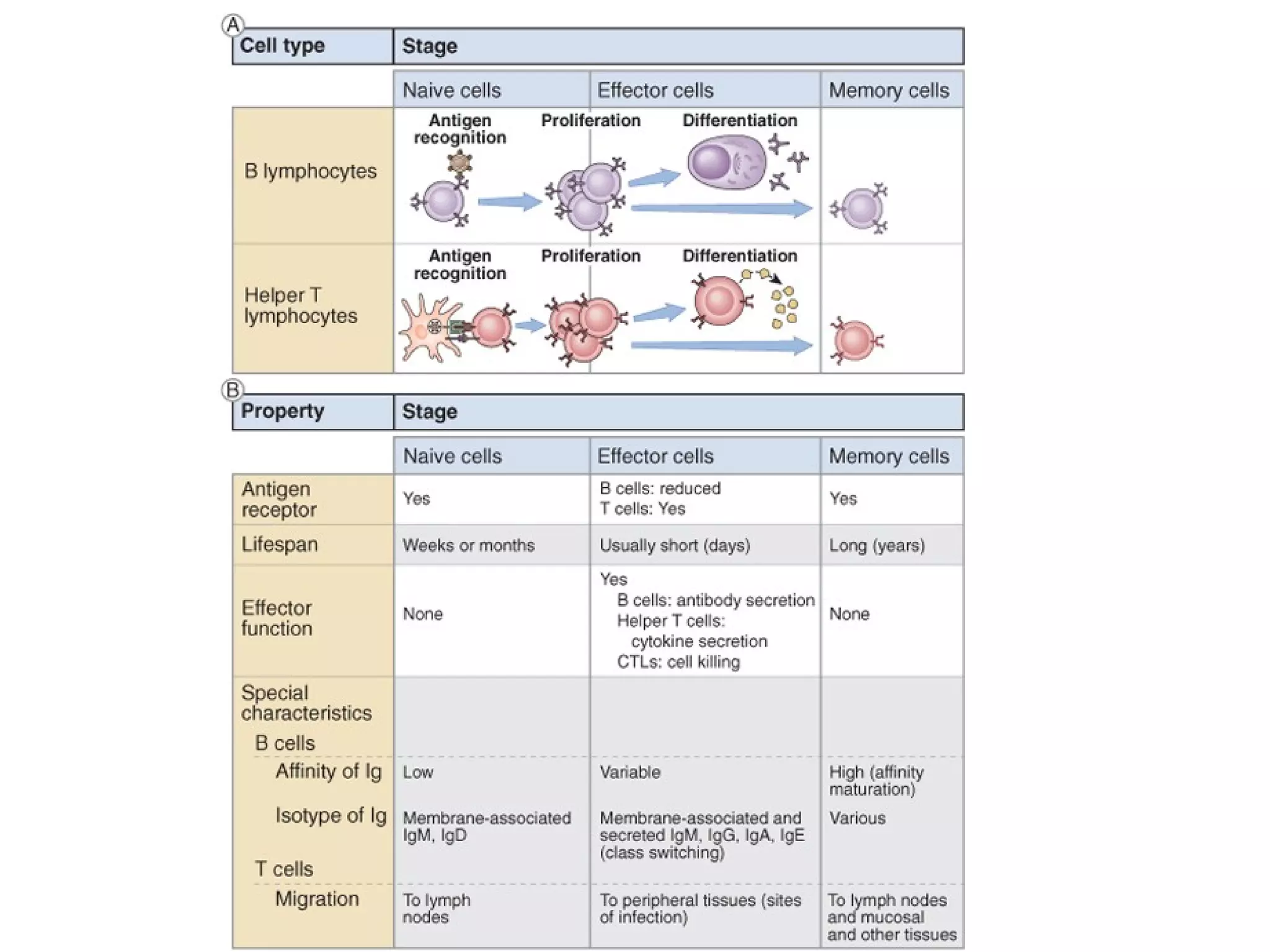
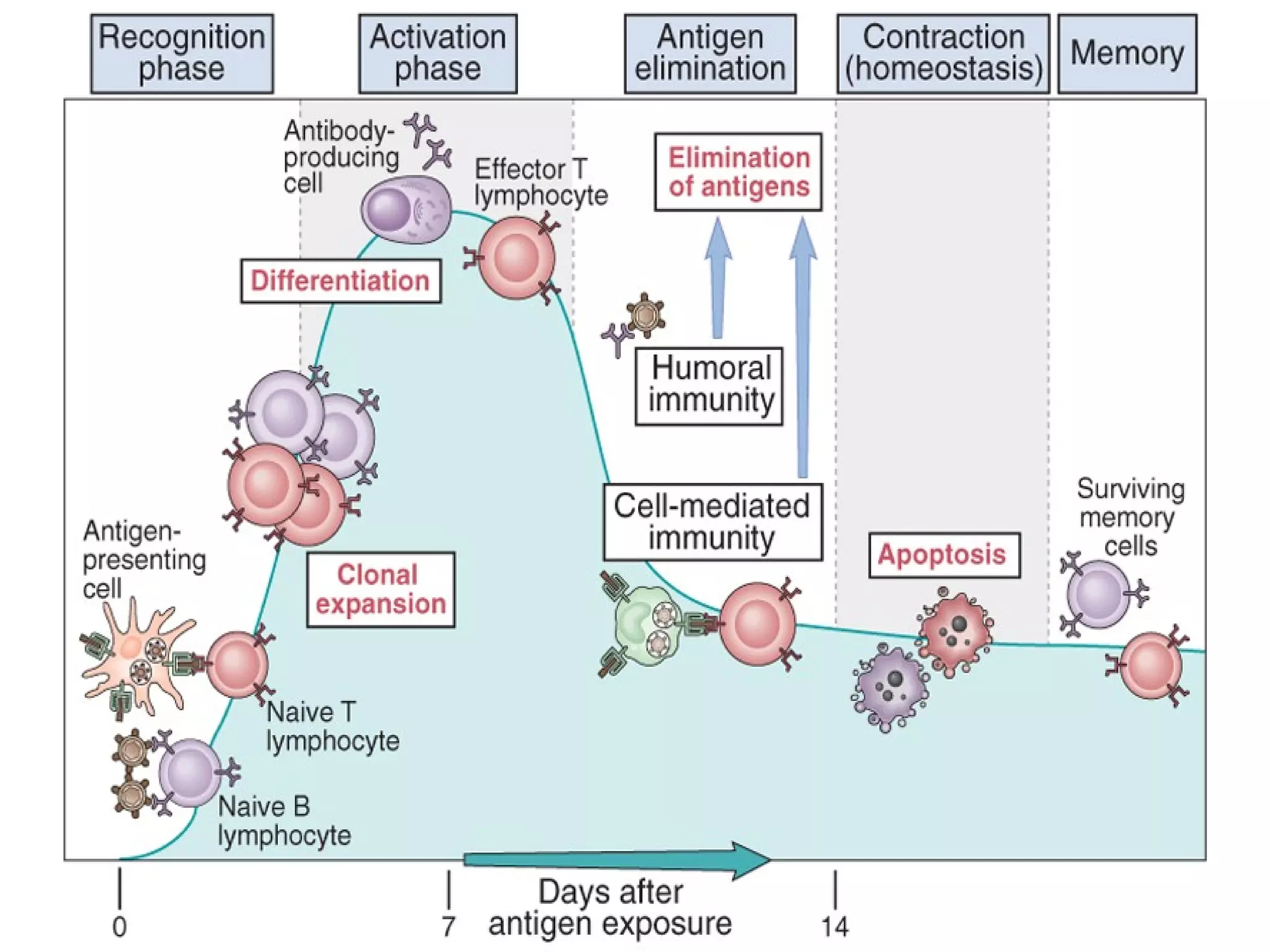
- Adaptive immunity includes humoral immunity from B cells producing antibodies and cellular immunity from T cells killing infected cells.
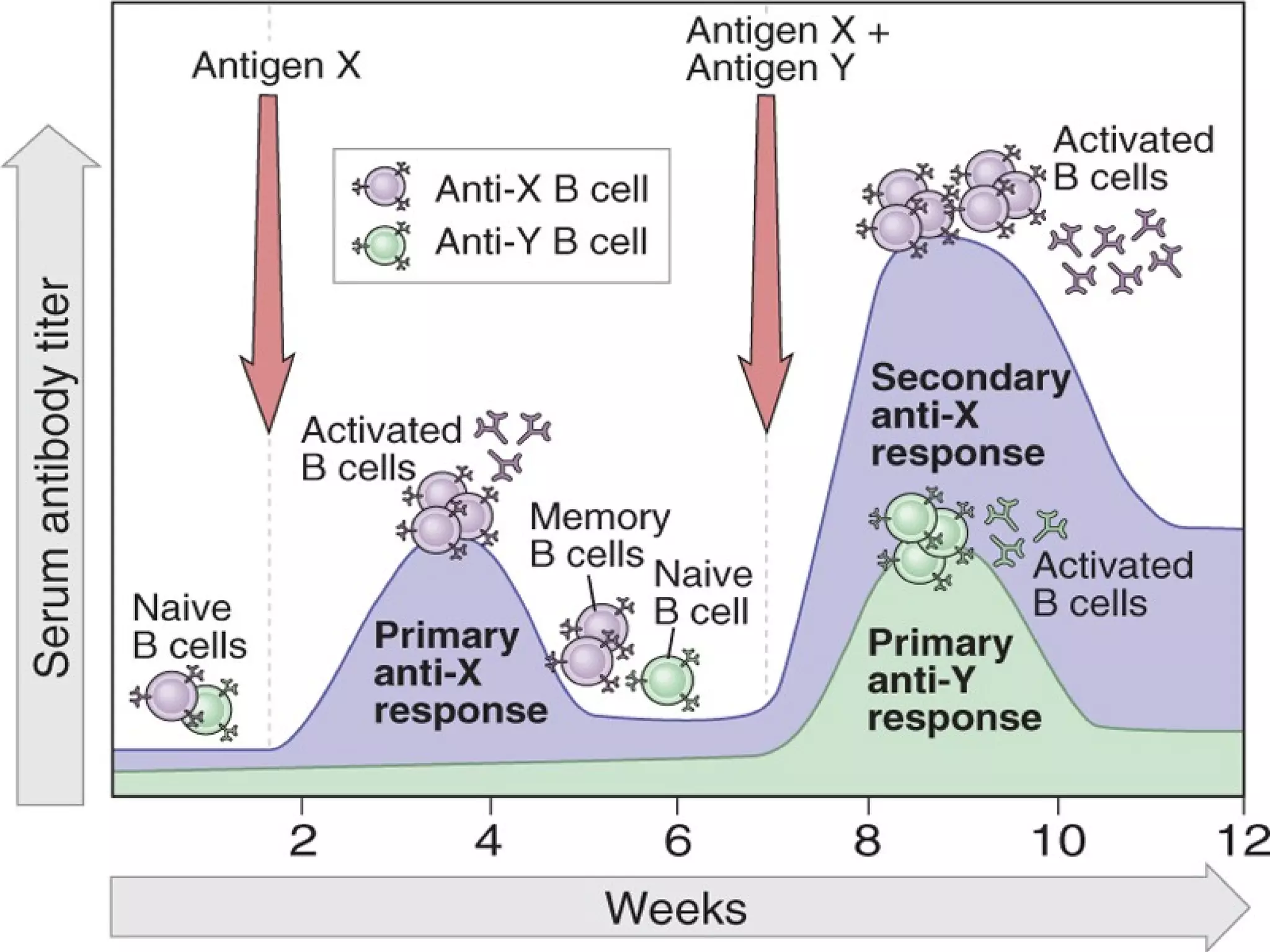
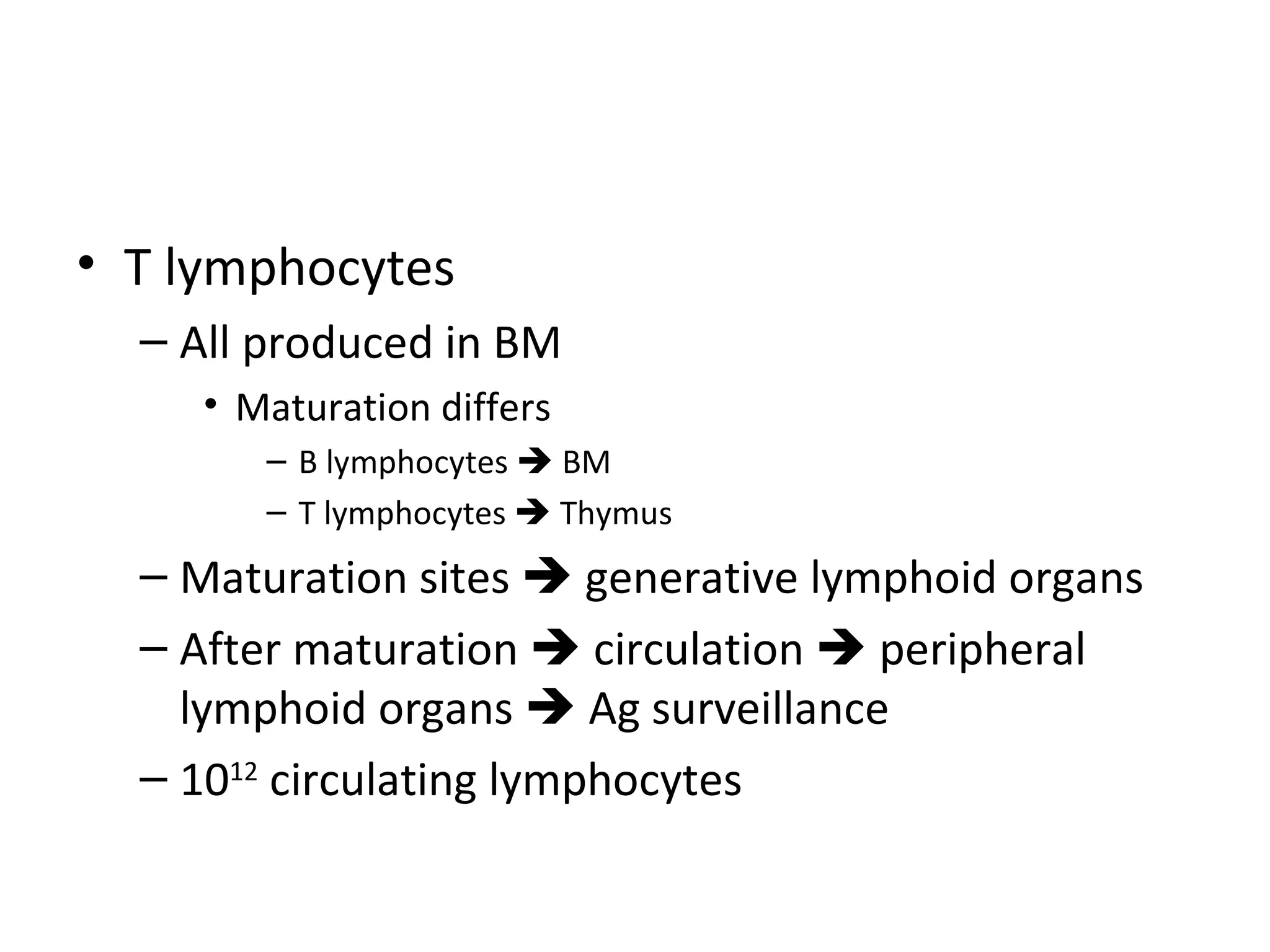
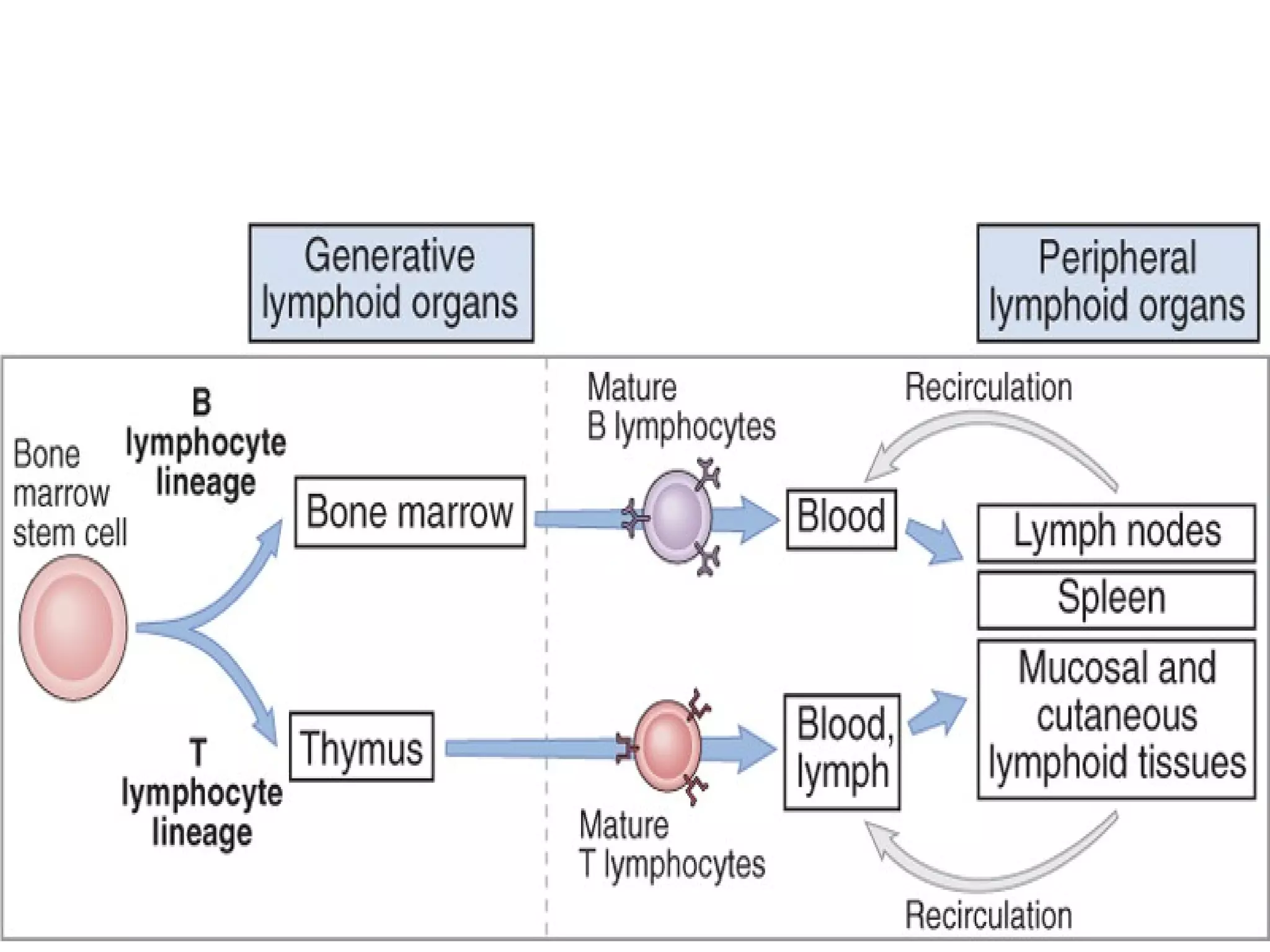
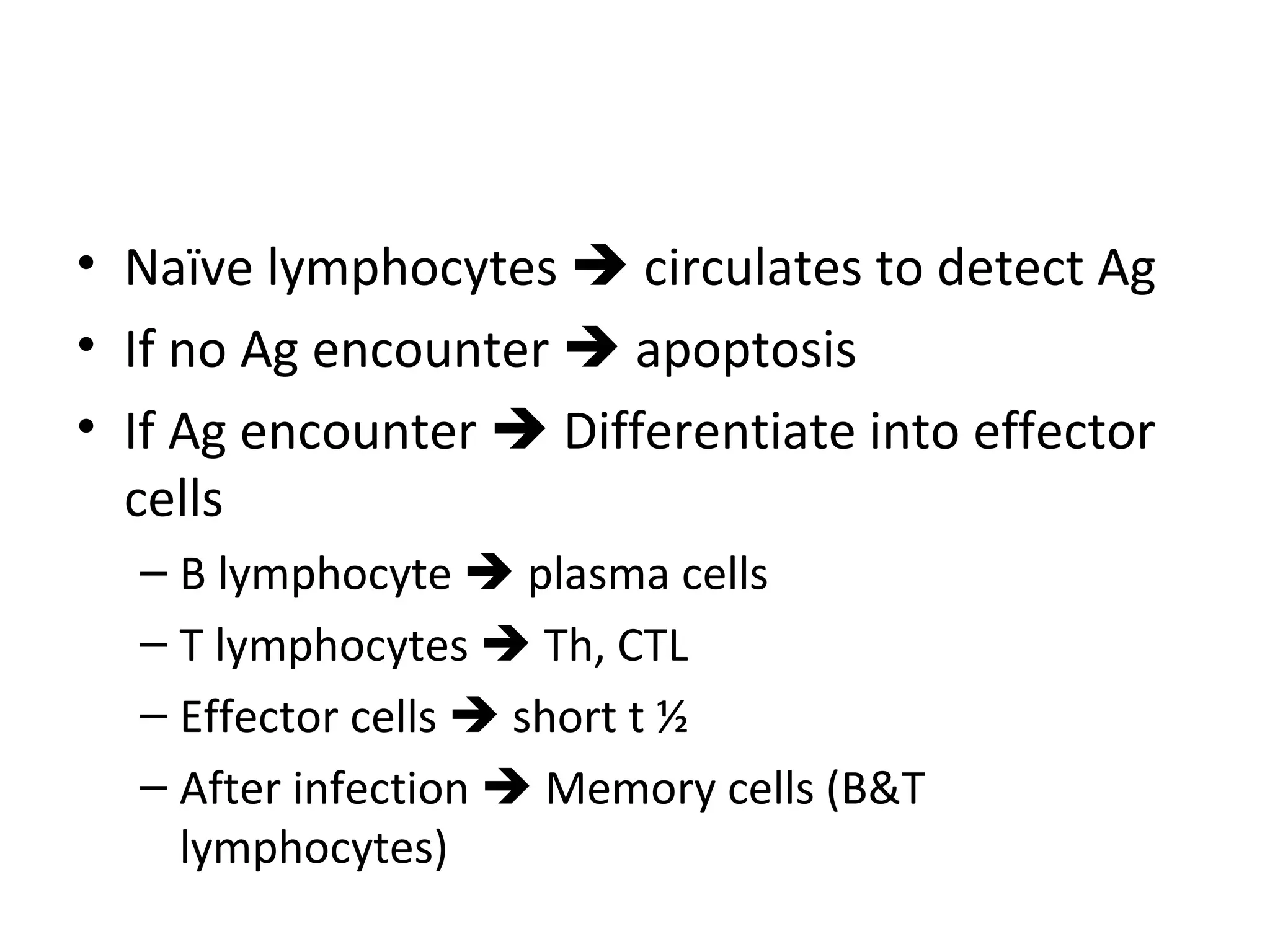
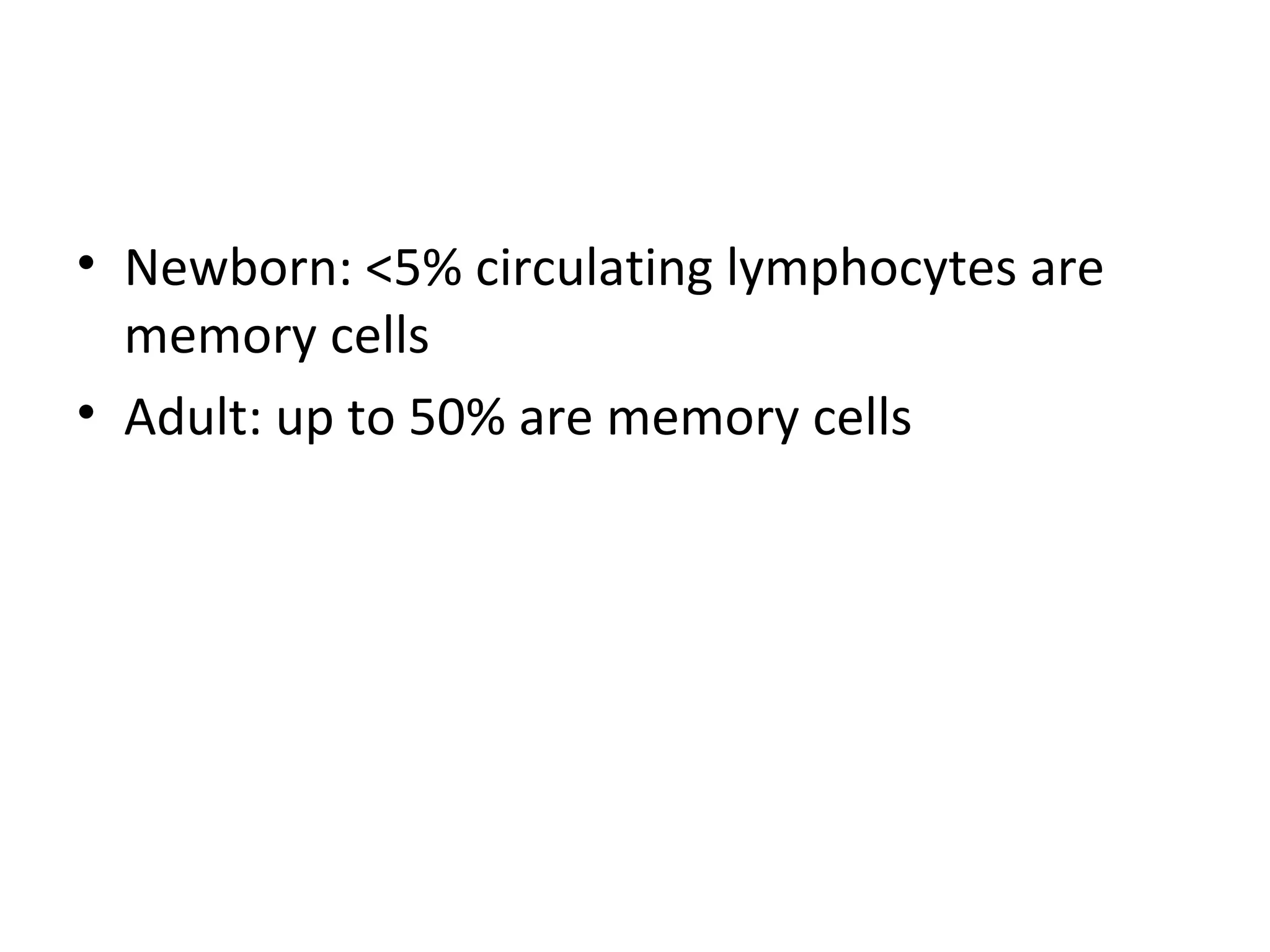
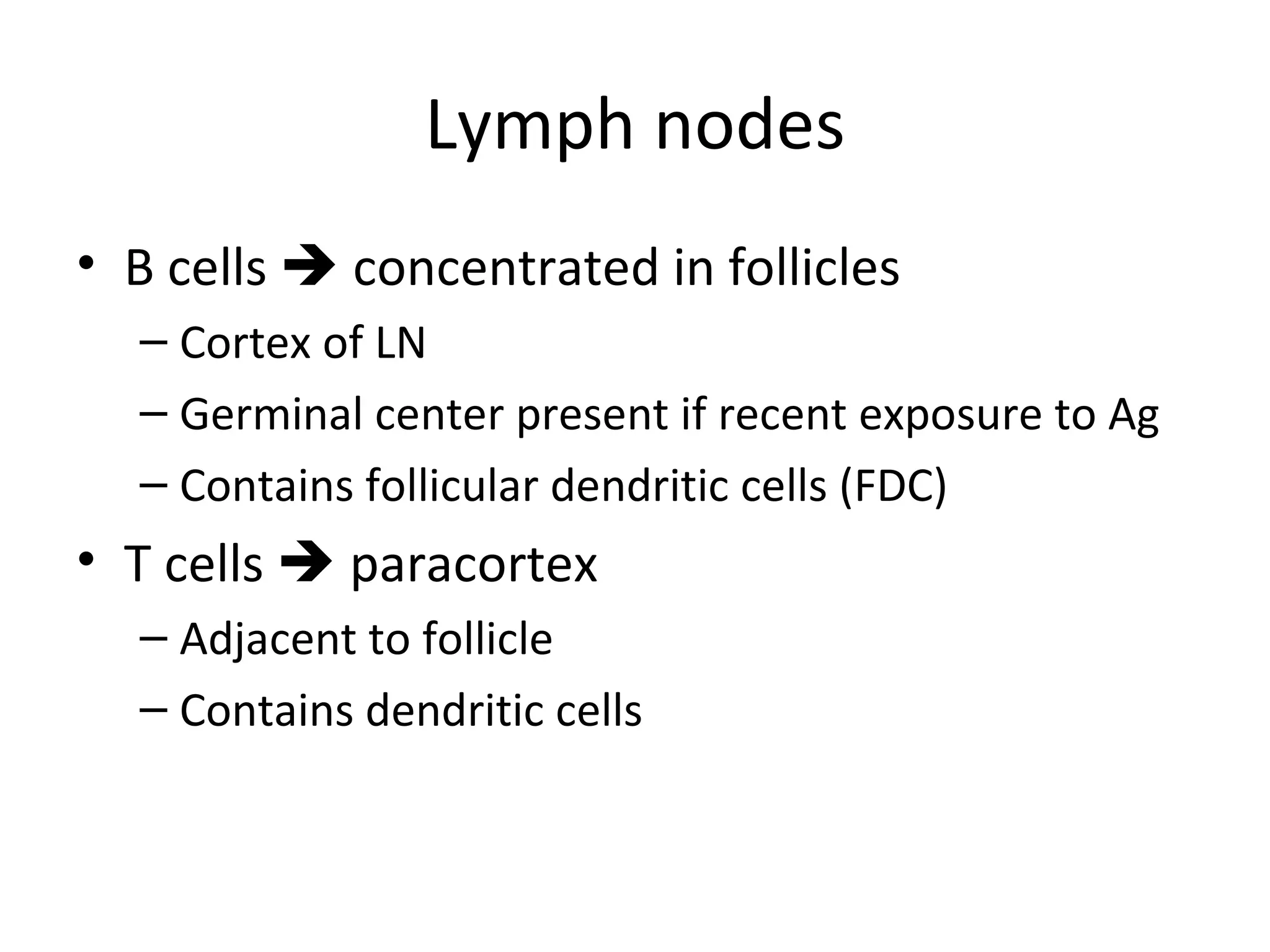
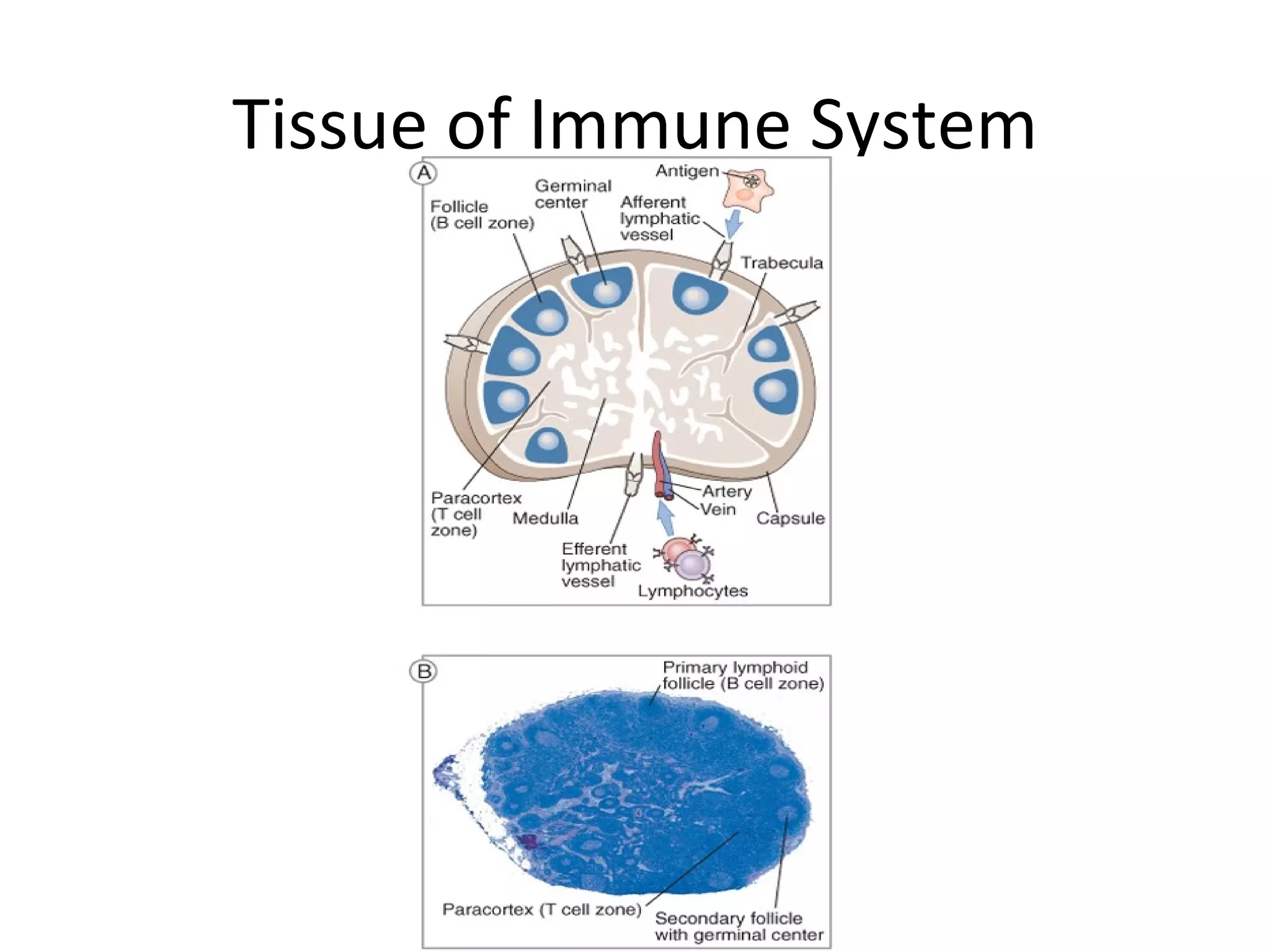
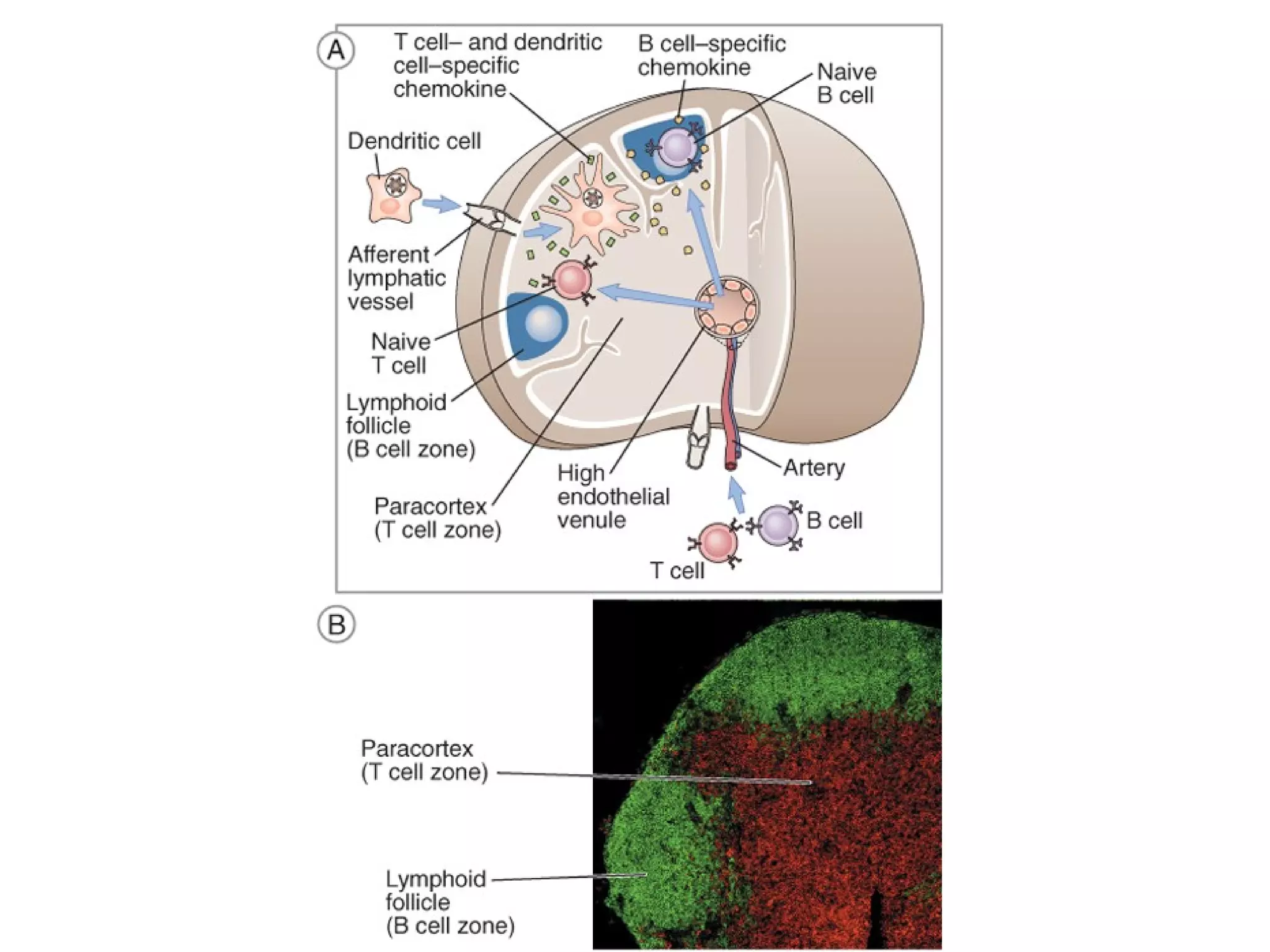
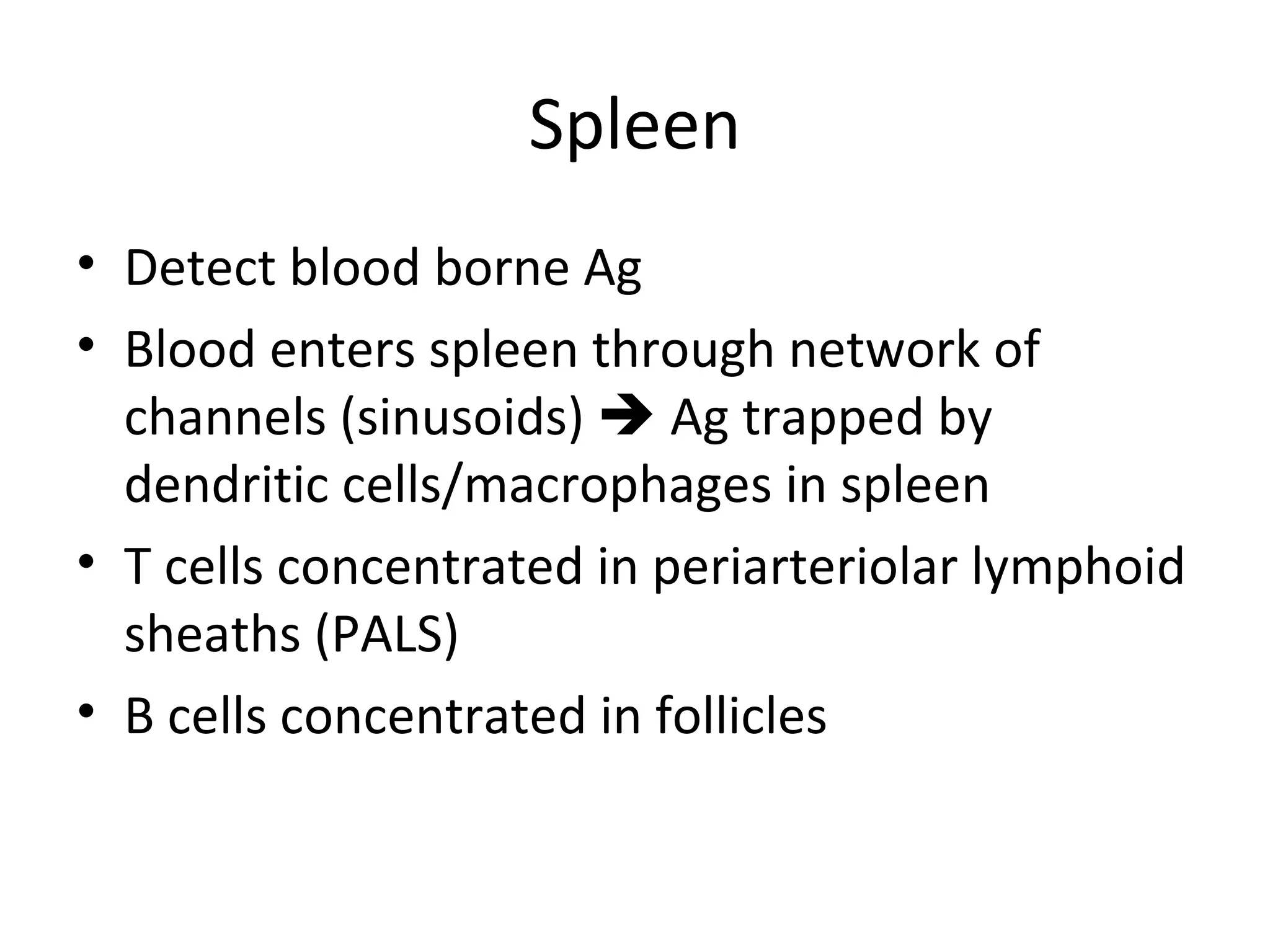
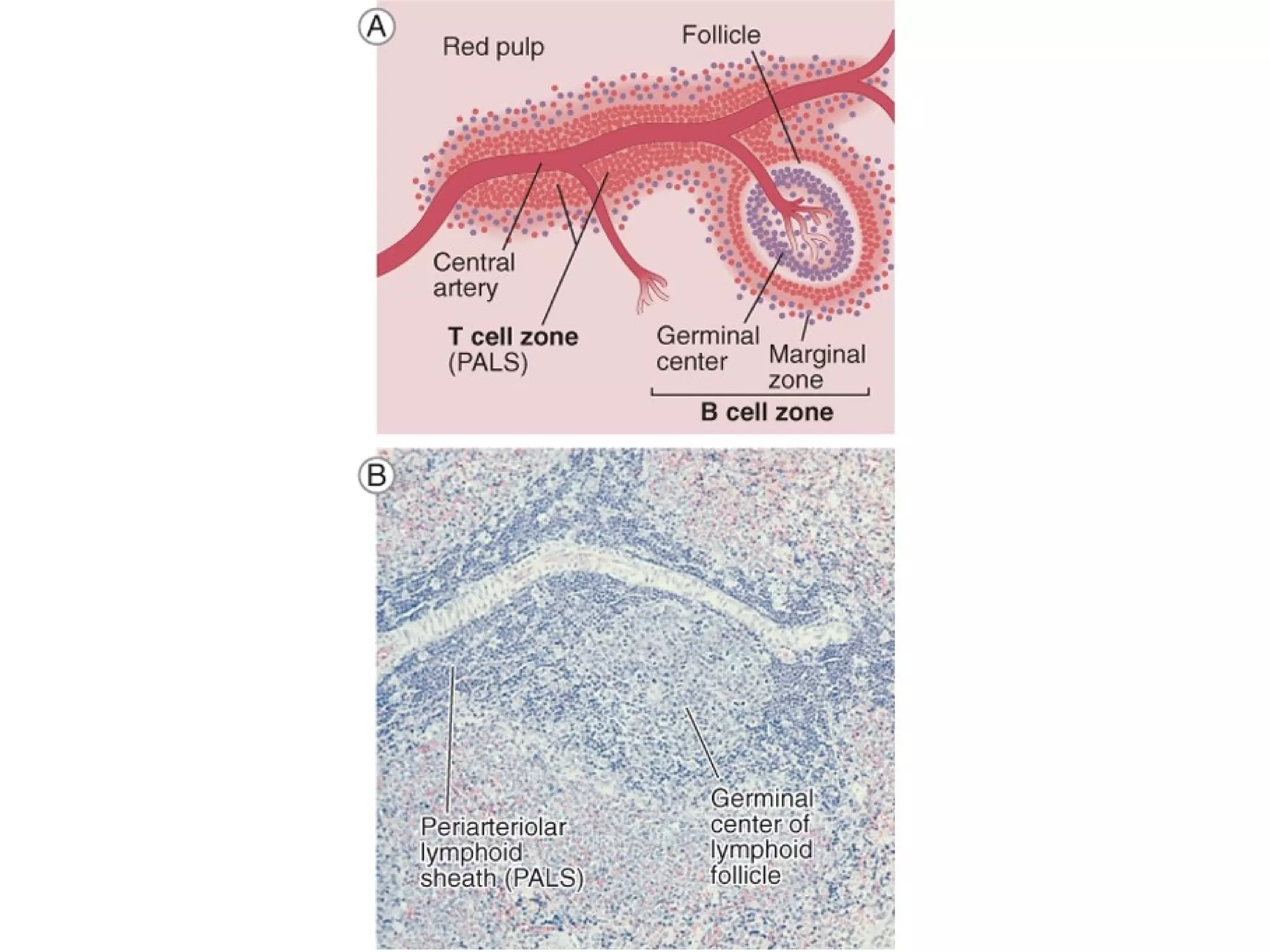
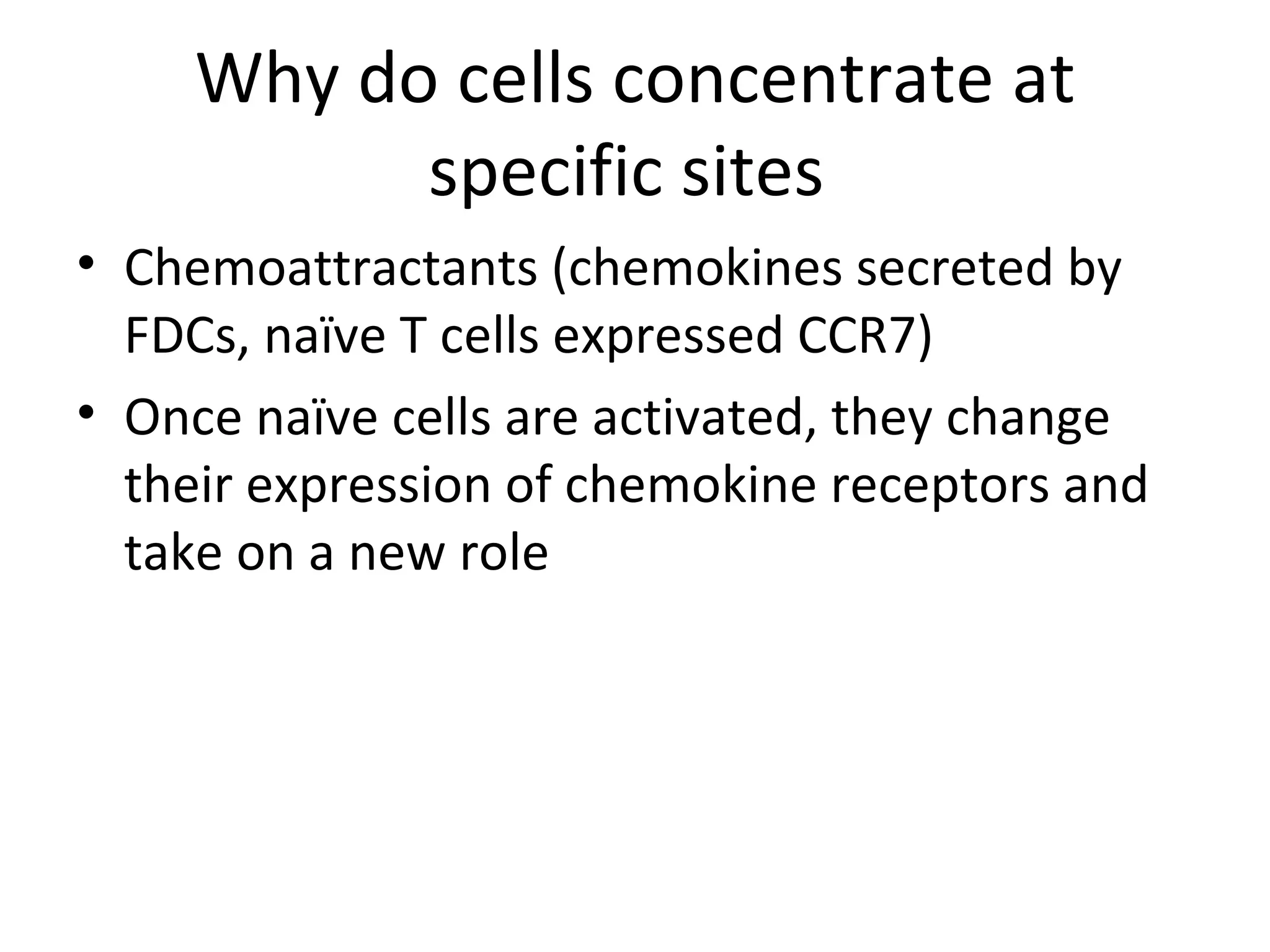
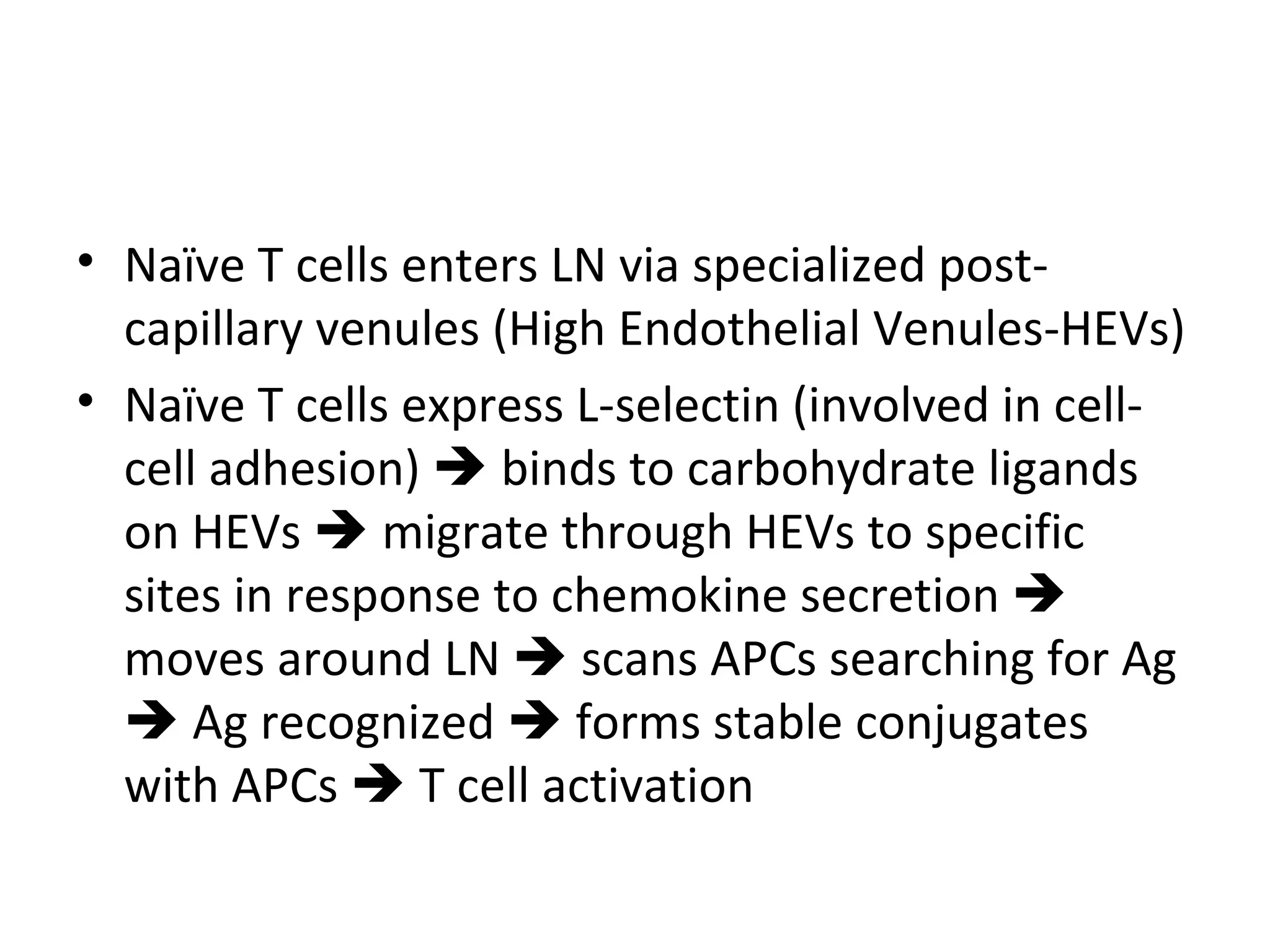
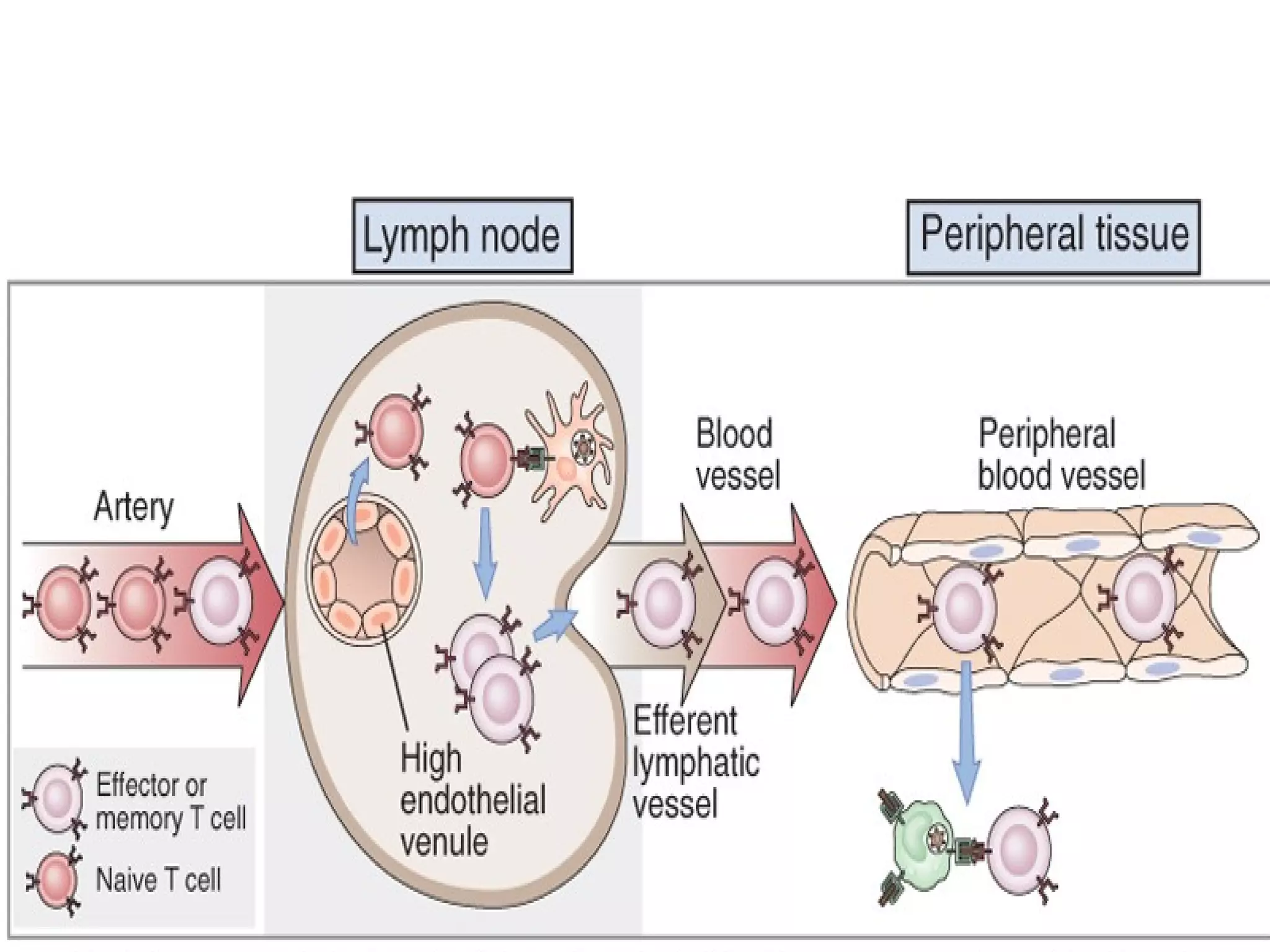
- Lymphocytes circulate and are concentrated in lymphoid tissues like lymph nodes and spleen to scan for pathogens using antigen presenting cells. Memory lymphocytes provide faster responses upon reexposure.