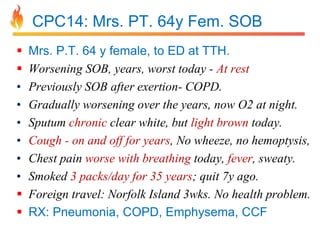
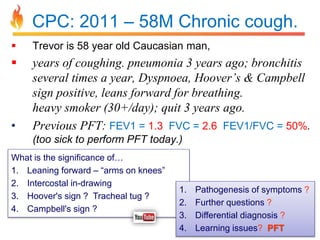
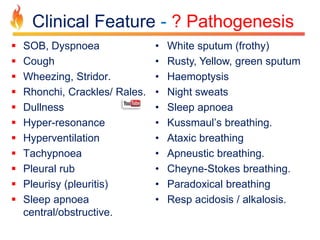
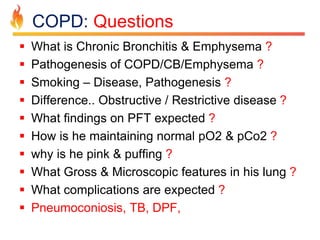
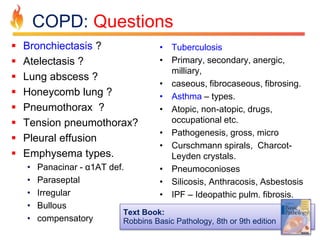
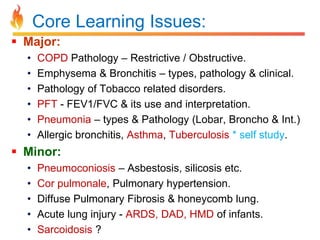
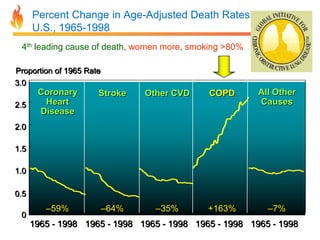
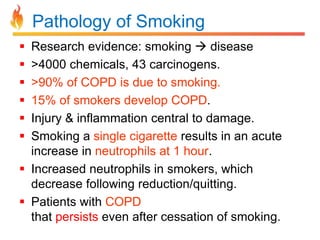
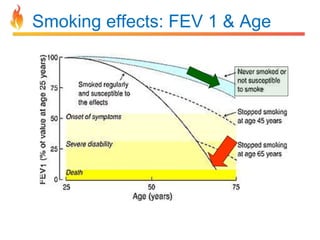
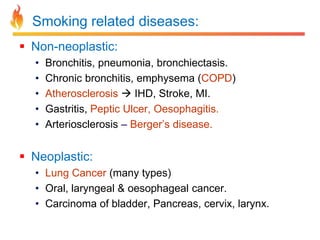
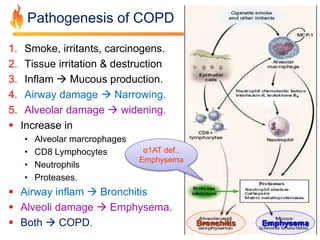
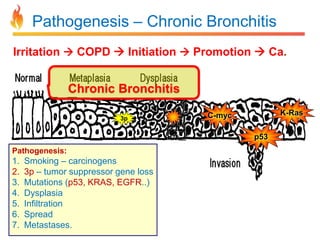
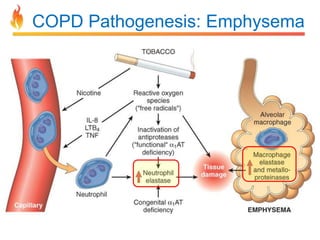
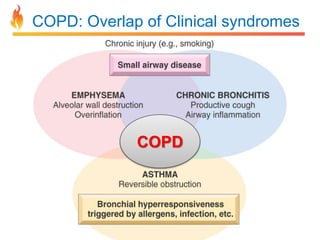
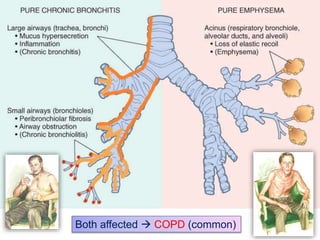
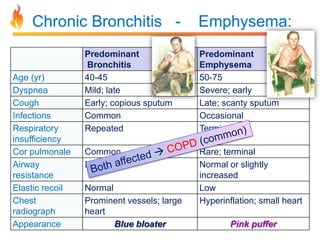
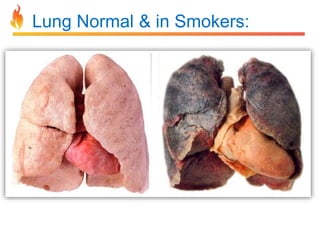
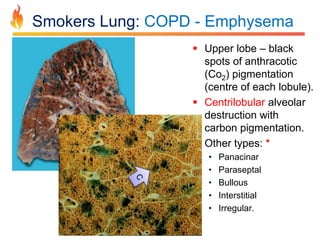
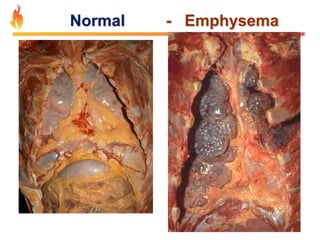
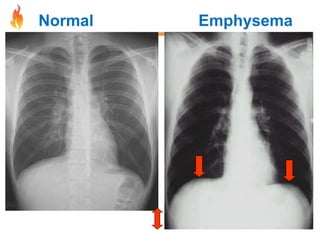
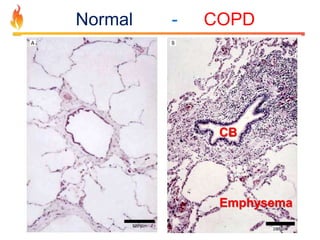
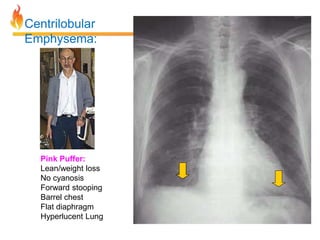
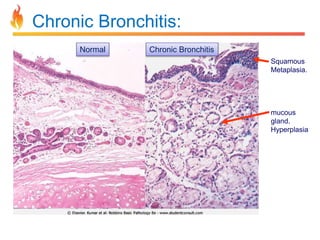
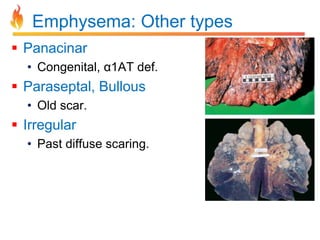
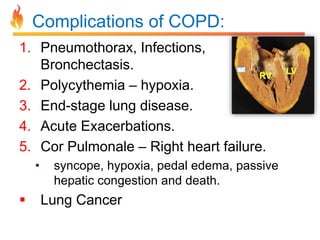
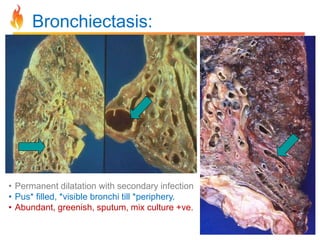
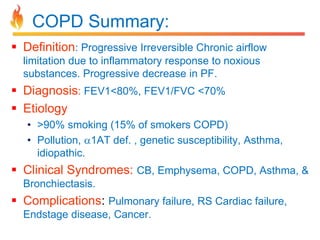
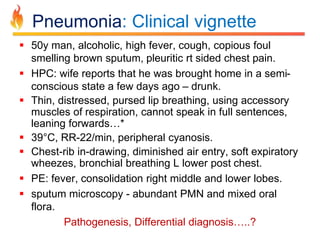
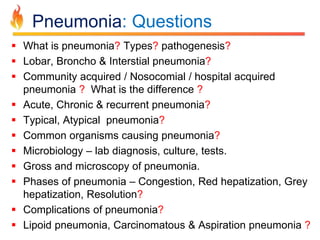
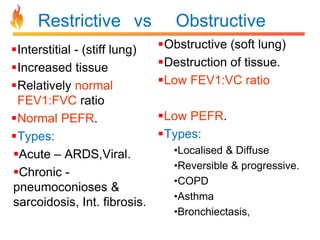
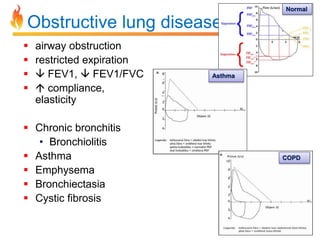
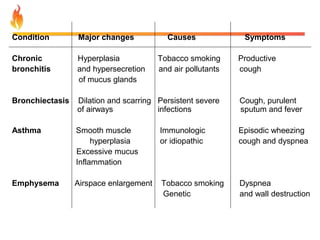
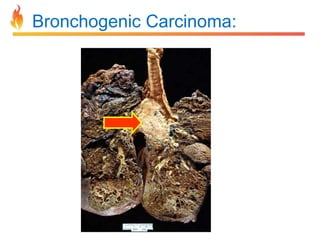
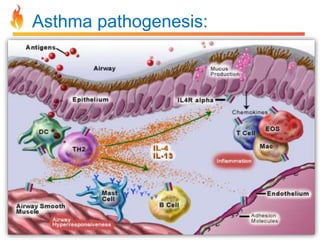
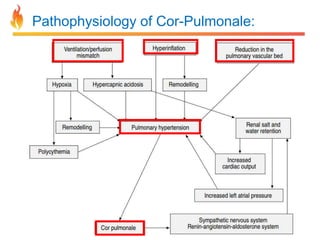
Within the document are discussions of chronic obstructive pulmonary disease (COPD) and pneumonia. It summarizes the pathogenesis of COPD as being caused by long-term smoke and irritant inhalation leading to airway and lung tissue damage, inflammation, and impaired lung function over time. Emphysema specifically involves destruction of alveoli walls, while chronic bronchitis involves inflammation of the airways. Complications discussed include respiratory infections, lung cancer, and cor pulmonale. Pneumonia is also briefly discussed through a clinical vignette of an alcoholic man presenting with fever, cough, and signs of consolidation on exam.