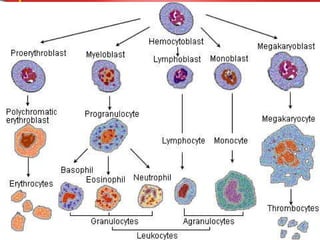
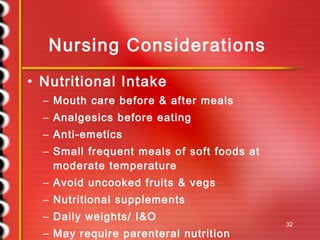
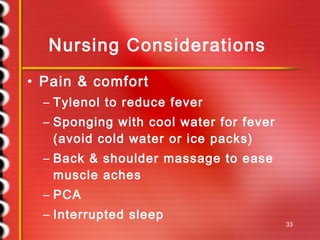
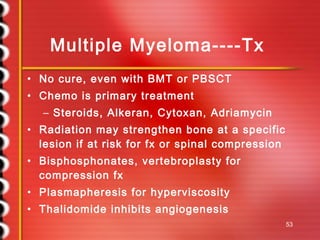
This document provides an overview of cancers of the hematopoietic system, including leukemia and lymphoma. It discusses the etiology, pathophysiology, signs and symptoms, diagnostic findings, treatment approaches, nursing considerations, and outcomes for various types of leukemia (acute myeloid leukemia, chronic myelogenous leukemia, acute lymphocytic leukemia, chronic lymphocytic leukemia) and lymphomas (Hodgkin's lymphoma, non-Hodgkin's lymphoma, multiple myeloma). It also covers bone marrow transplantation as a treatment option.