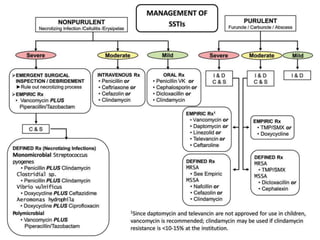
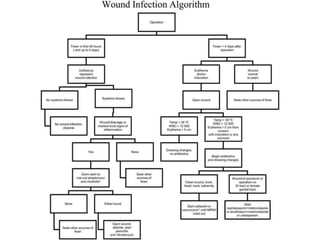
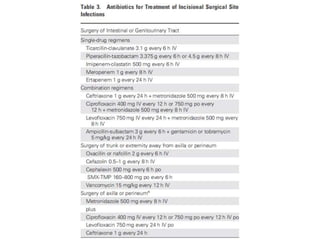
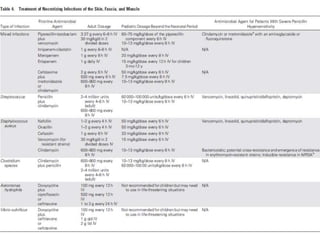
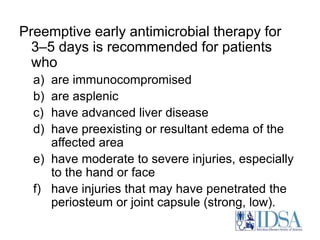
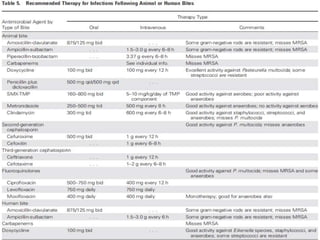
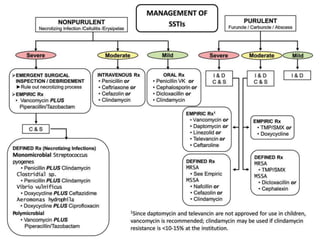
The IDSA guidelines provide comprehensive recommendations for the diagnosis and management of skin and soft tissue infections (SSTIs) including purulent and nonpurulent infections, emphasizing the importance of proper evaluation, including cultures, and appropriate antibiotic usage. Key treatment strategies include incision and drainage for abscesses and carbuncles, systemic antibiotics for severe infections, and careful management of recurrent infections with prophylactic measures. Surgical site infections and complications like necrotizing fasciitis necessitate urgent surgical intervention, and the guidelines suggest specific antimicrobial regimens based on infection severity and risk factors.