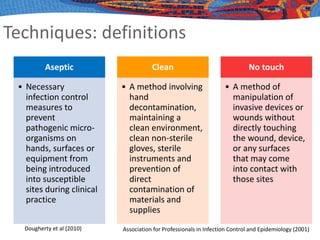
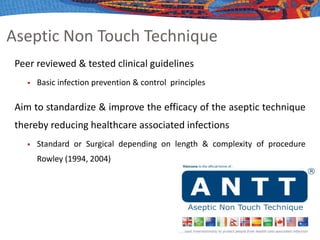
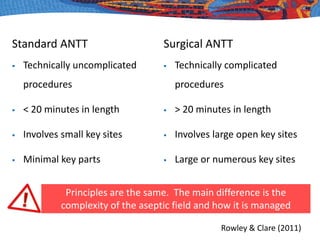
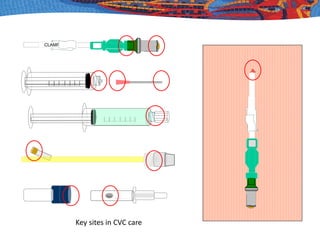
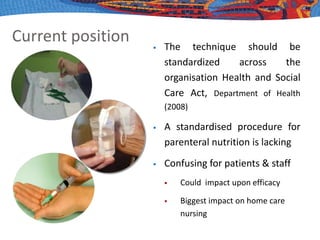
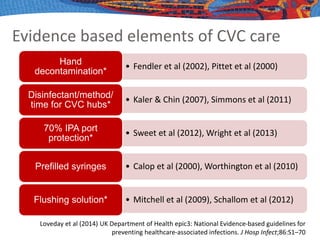
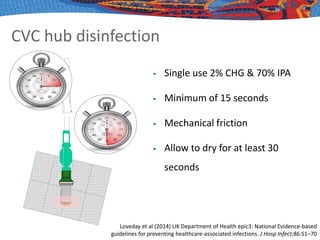
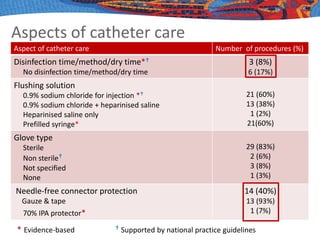
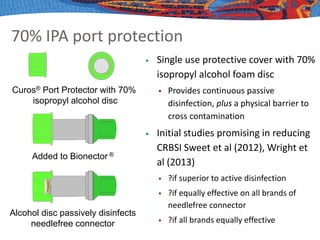
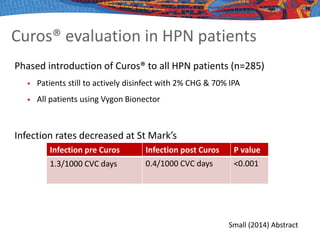
This document discusses aseptic technique for central venous catheter care. It defines asepsis and aseptic technique, and describes the evidence base for various aspects of catheter care. Key evidence-based elements that should be included in any standardized technique are hand decontamination with alcohol, disinfecting catheter hubs with chlorhexidine for at least 15 seconds, using prefilled syringes, flushing with saline, and protecting ports with isopropyl alcohol discs. Outcomes like infection rates can assess the efficacy of techniques, but definitions and diagnostic methods vary, making direct comparisons difficult. Standardizing catheter care procedures according to evidence-based principles could help improve outcomes.