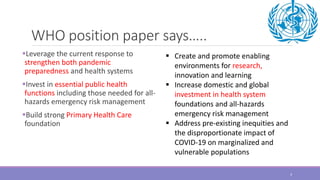
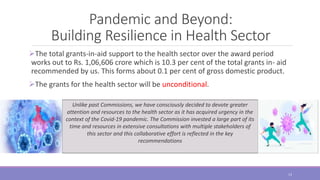
The document discusses recommendations from the 15th Finance Commission (XV FC) on building resilience in India's health sector in light of the COVID-19 pandemic. Some key points:
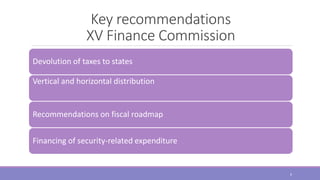
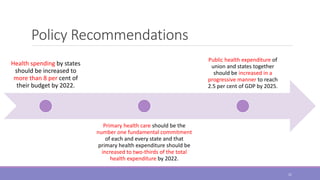
- The XV FC recommends increasing public health expenditure to reach 2.5% of GDP by 2025 and prioritizing primary healthcare.
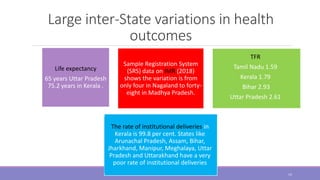
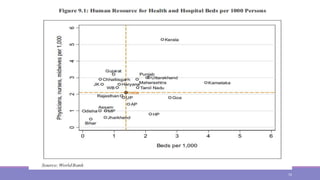
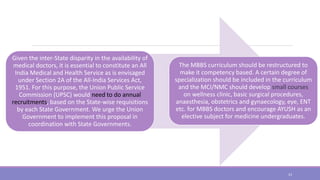
- It acknowledges issues like lack of infrastructure, inter-state disparities in health outcomes, and out-of-pocket medical expenses pushing people into poverty.
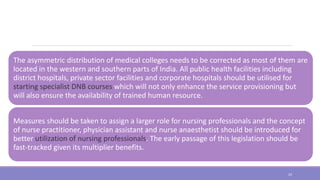
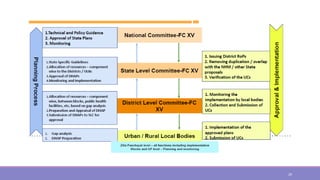
- Policy recommendations include increasing state health budgets, reforming centrally-sponsored schemes, constituting an all-India health service, and restructuring medical education.
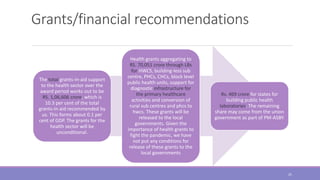
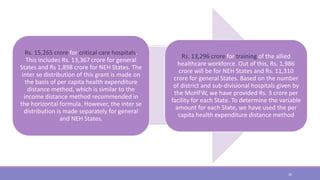
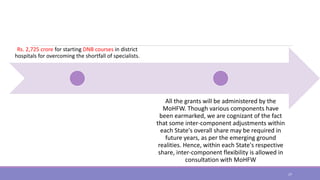
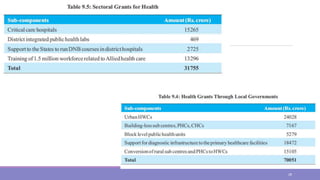
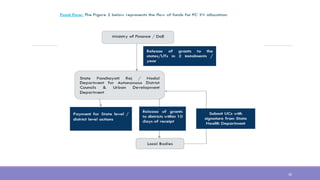
- The XV FC proposes unconditional health grants totaling Rs.