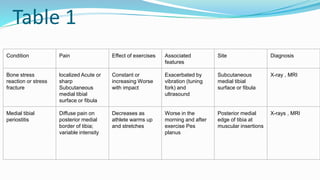
The document discusses shin pain in athletes, which can be caused by bone stress, vascular issues, inflammation, nerve entrapment, and biomechanical factors related to foot type; it provides details on the clinical perspectives, pain sites, effects of exercise, and treatments for various conditions like stress fractures, periostitis, and compartment syndrome; treatments discussed include rest, bracing, electrical stimulation, ultrasound, stretching, orthotics, and physiotherapy.