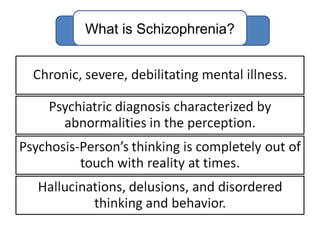
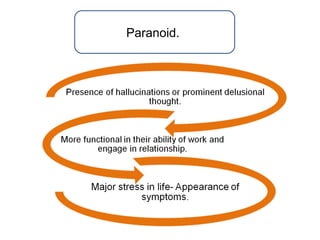
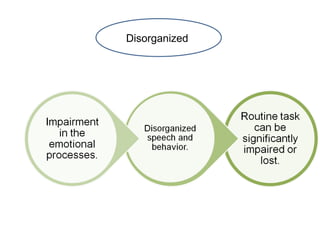
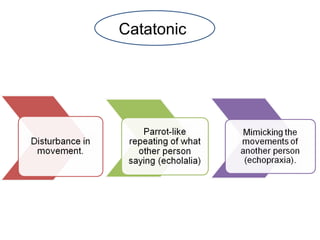
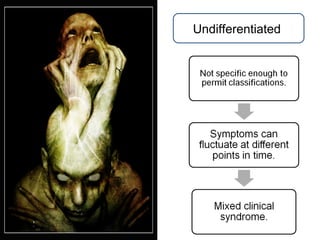
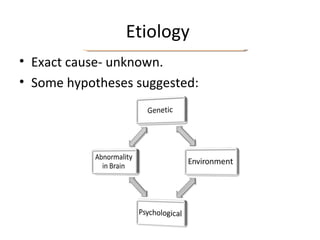
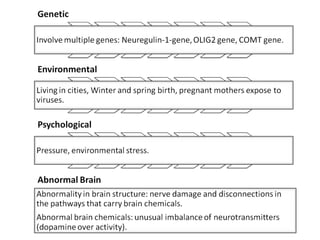
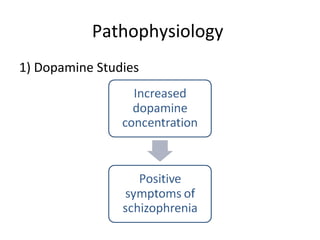
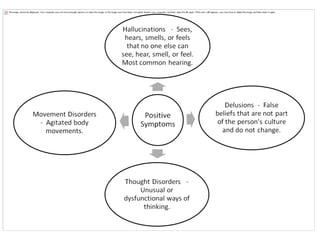
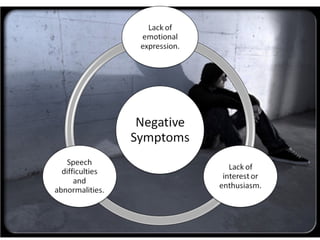
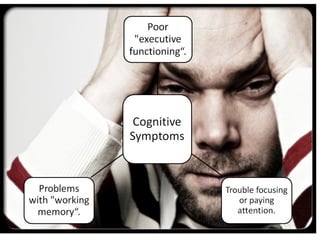
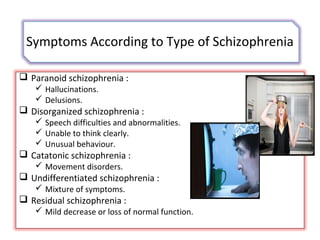
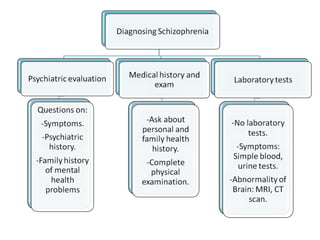
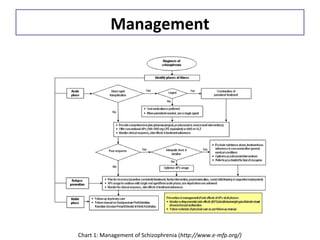
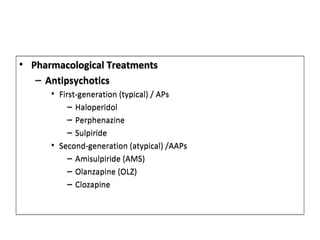
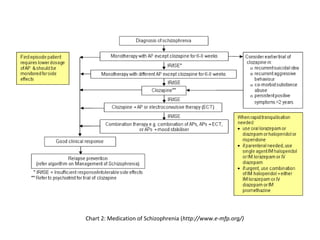
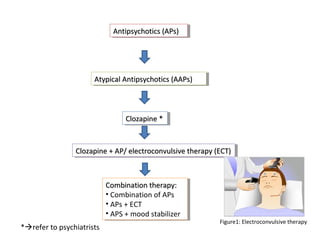
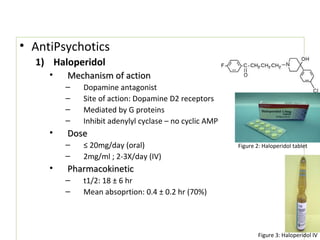
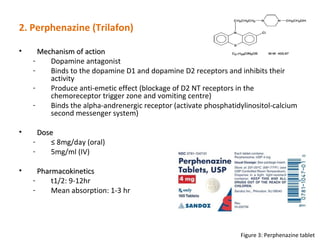
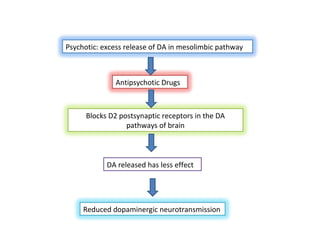
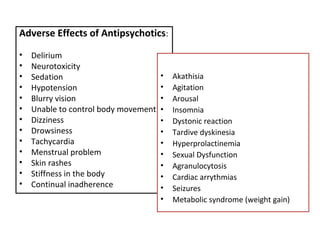
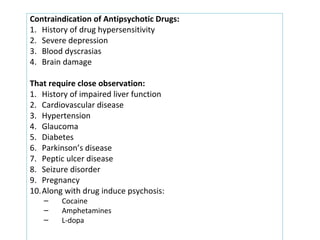
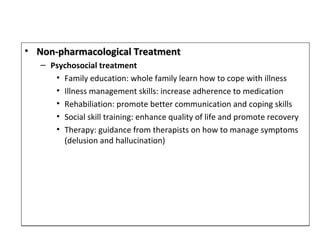
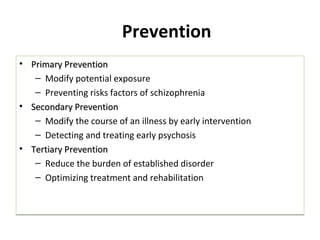
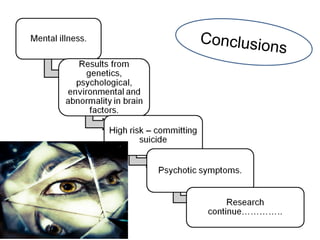
Schizophrenia is a mental disorder characterized by symptoms like hallucinations, delusions, and disorganized speech and behavior. It has no single known cause but may involve genetic and environmental factors. Treatment involves antipsychotic medications to manage symptoms as well as psychosocial therapies. Prevention strategies focus on reducing risk factors, early detection of psychosis, and improving long-term management of the disorder.