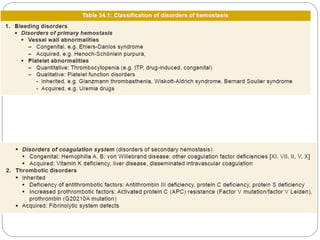
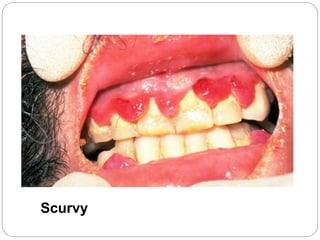
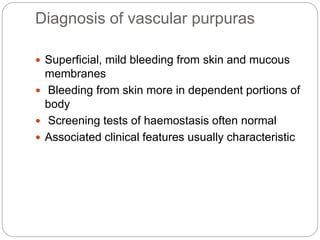
This document discusses bleeding disorders caused by vascular defects. It defines different types of hemorrhages including petechiae, purpura, and ecchymoses. It describes acquired vascular disorders such as senile purpura, scurvy, and vasculitis. Inherited disorders discussed are hereditary hemorrhagic telangiectasia and Ehlers-Danlos syndrome. The diagnostic approach for vascular purpuras is outlined.