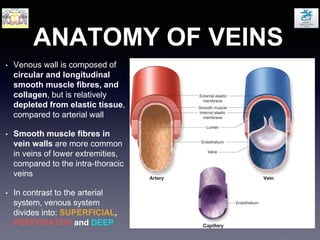
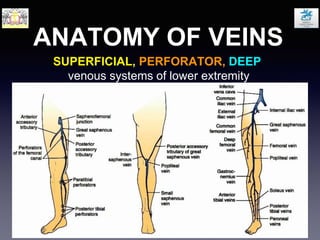
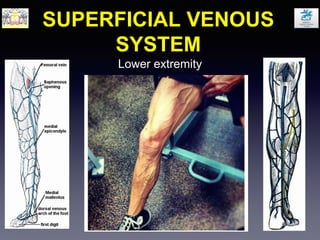
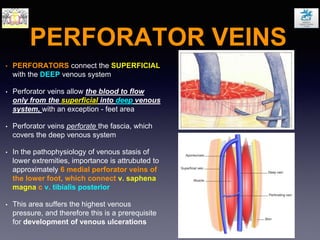
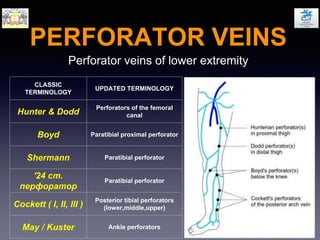
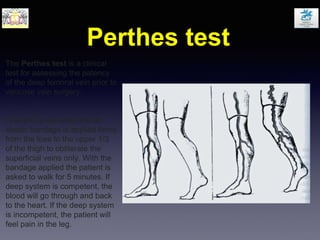
This document discusses varicose veins and their treatment. It begins by describing the anatomy and physiology of the venous system, including the roles of superficial, perforator, and deep veins as well as venous valves and the venous pump. It then discusses varicose veins specifically, including risk factors, classifications, and complications. Clinical features of varicose veins are outlined. The pathophysiology of varicose veins involves valve incompetence and chronic venous hypertension. Investigative tests for varicose veins are described. Surgical and non-surgical treatment options are presented.