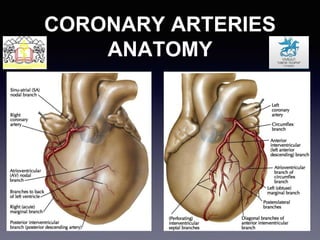
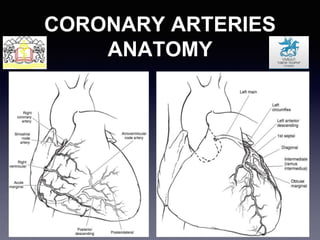
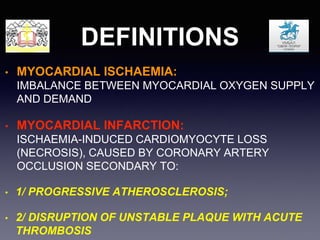
1. Coronary artery disease is caused by atherosclerosis developing in three stages, culminating in plaque rupture and thrombosis.
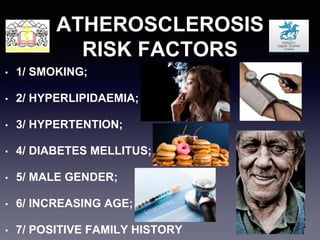
2. Risk factors for atherosclerosis and CAD include smoking, hyperlipidemia, hypertension, diabetes, male gender, increasing age, and family history.
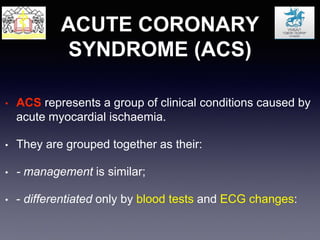
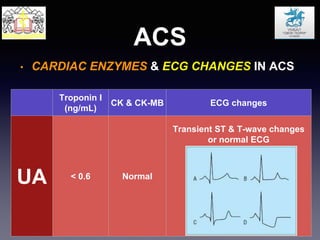
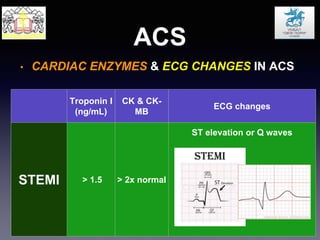
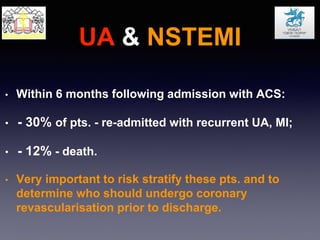
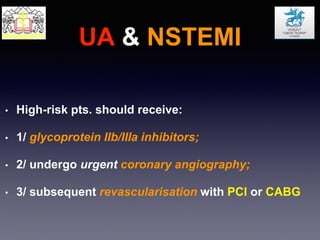
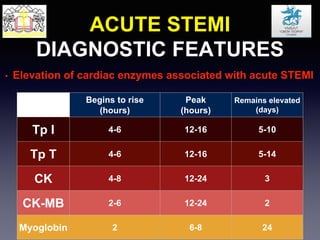
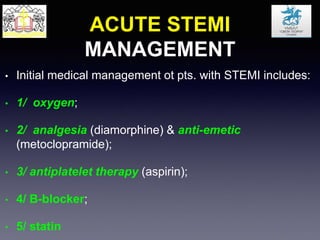
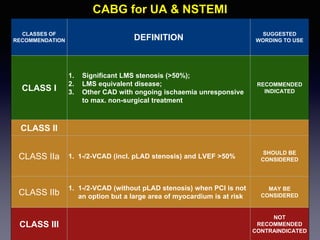
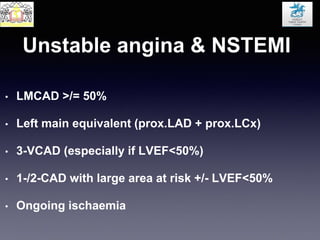
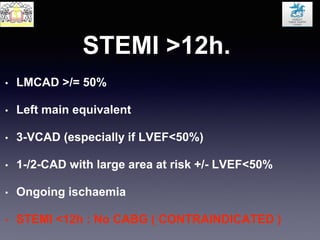
3. Acute coronary syndromes include unstable angina, NSTEMI, and STEMI, differentiated by cardiac enzymes and ECG changes. High-risk patients with ongoing symptoms should receive urgent angiography and revascularization.