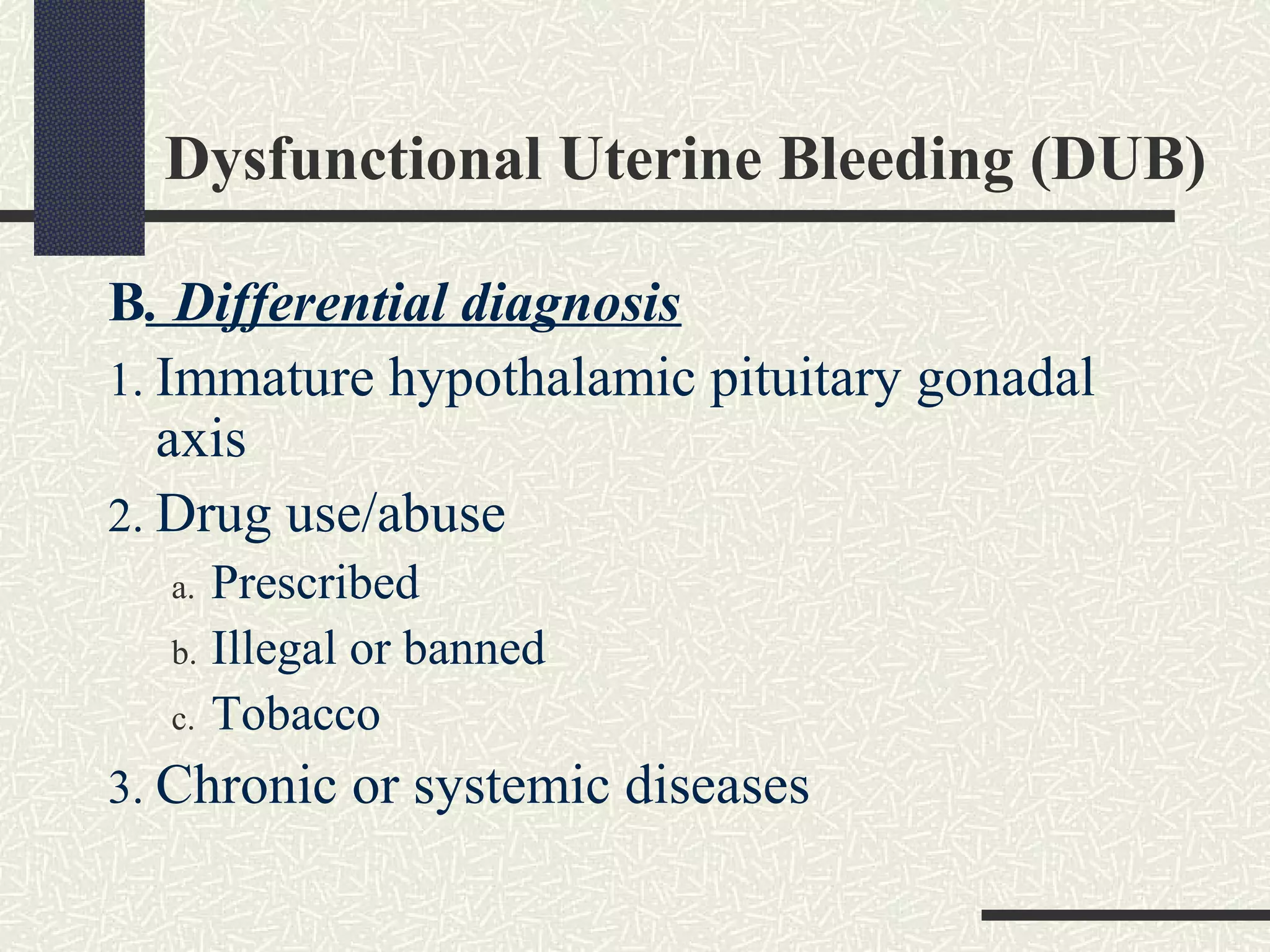
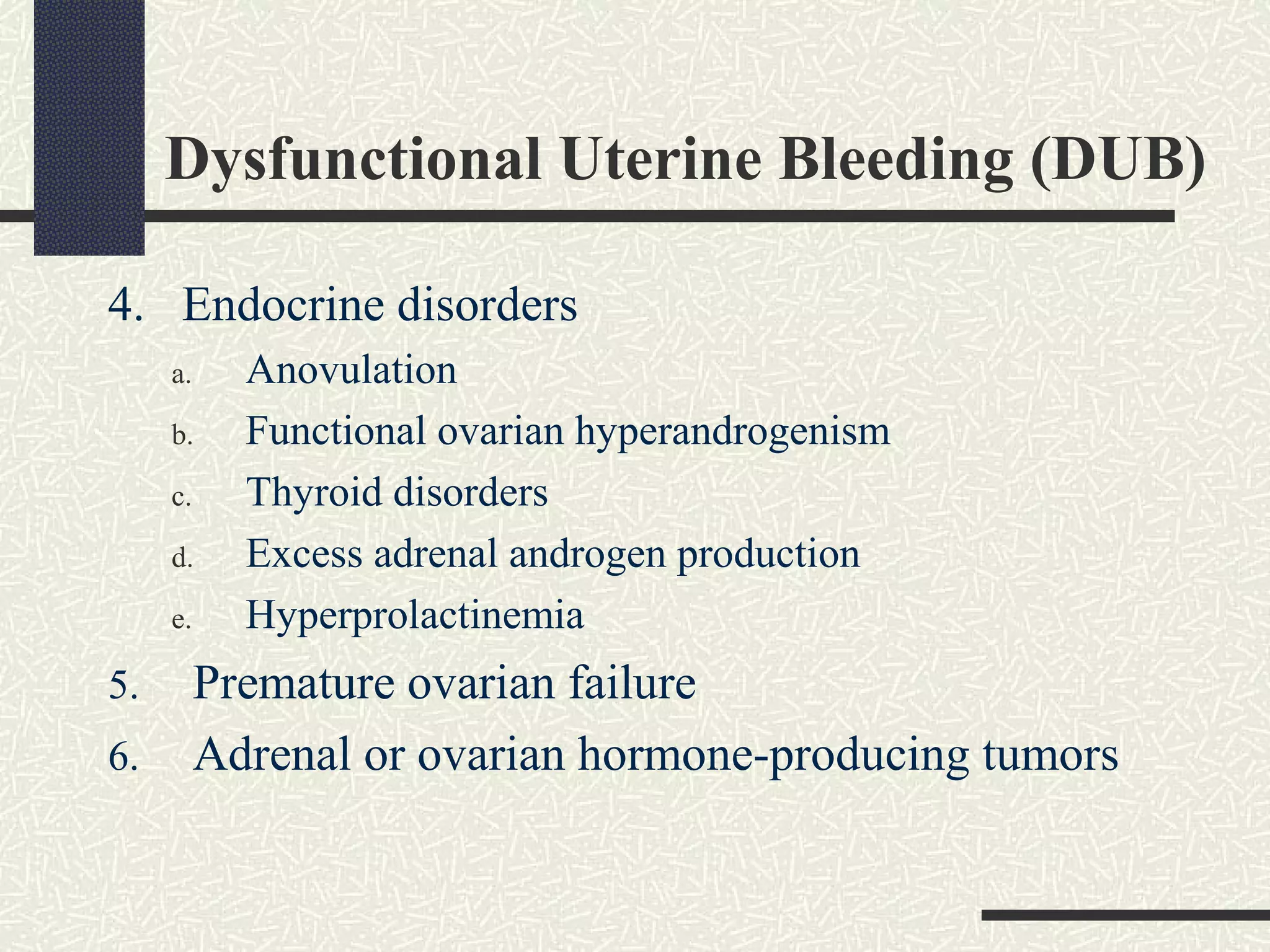
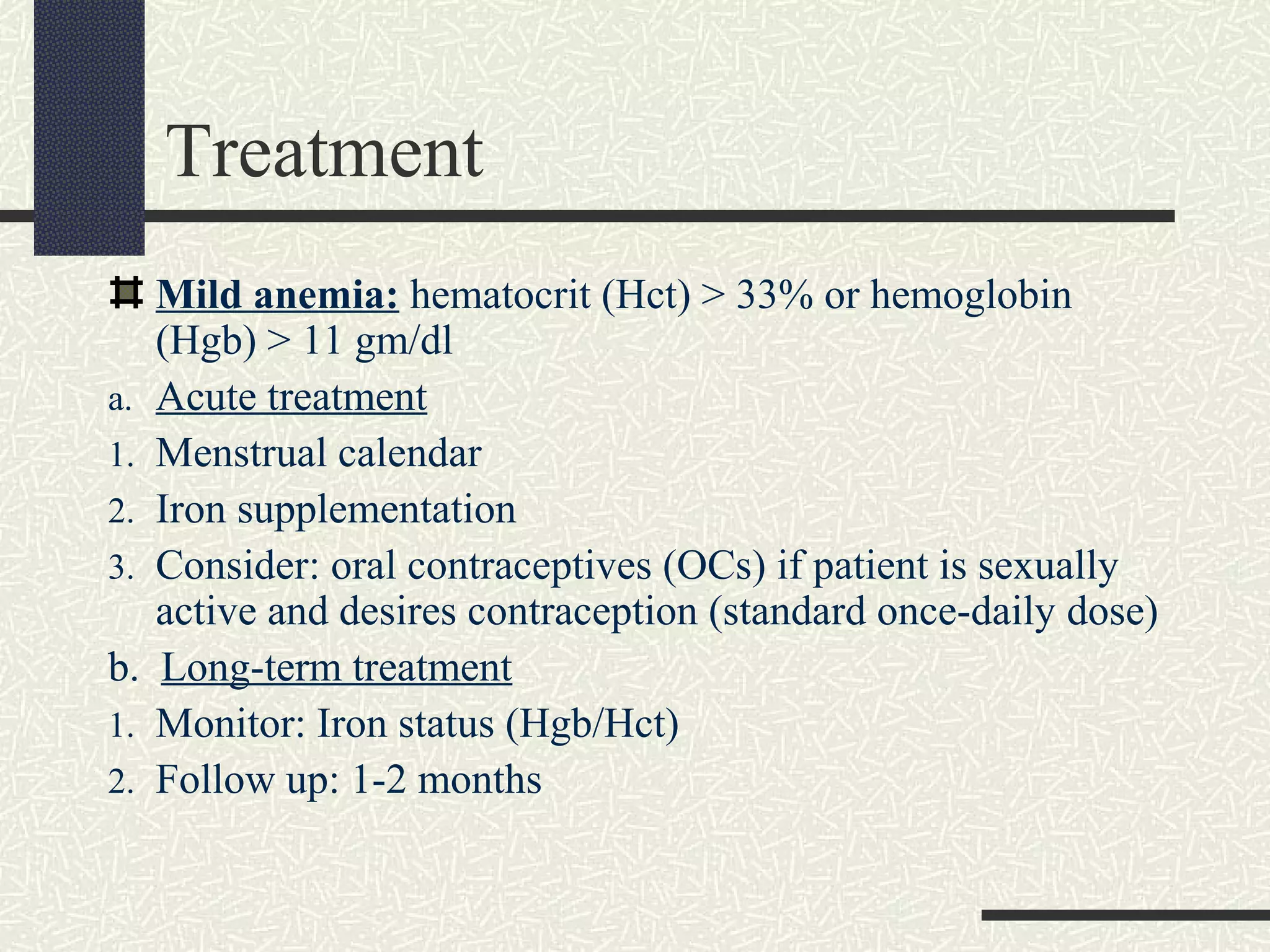
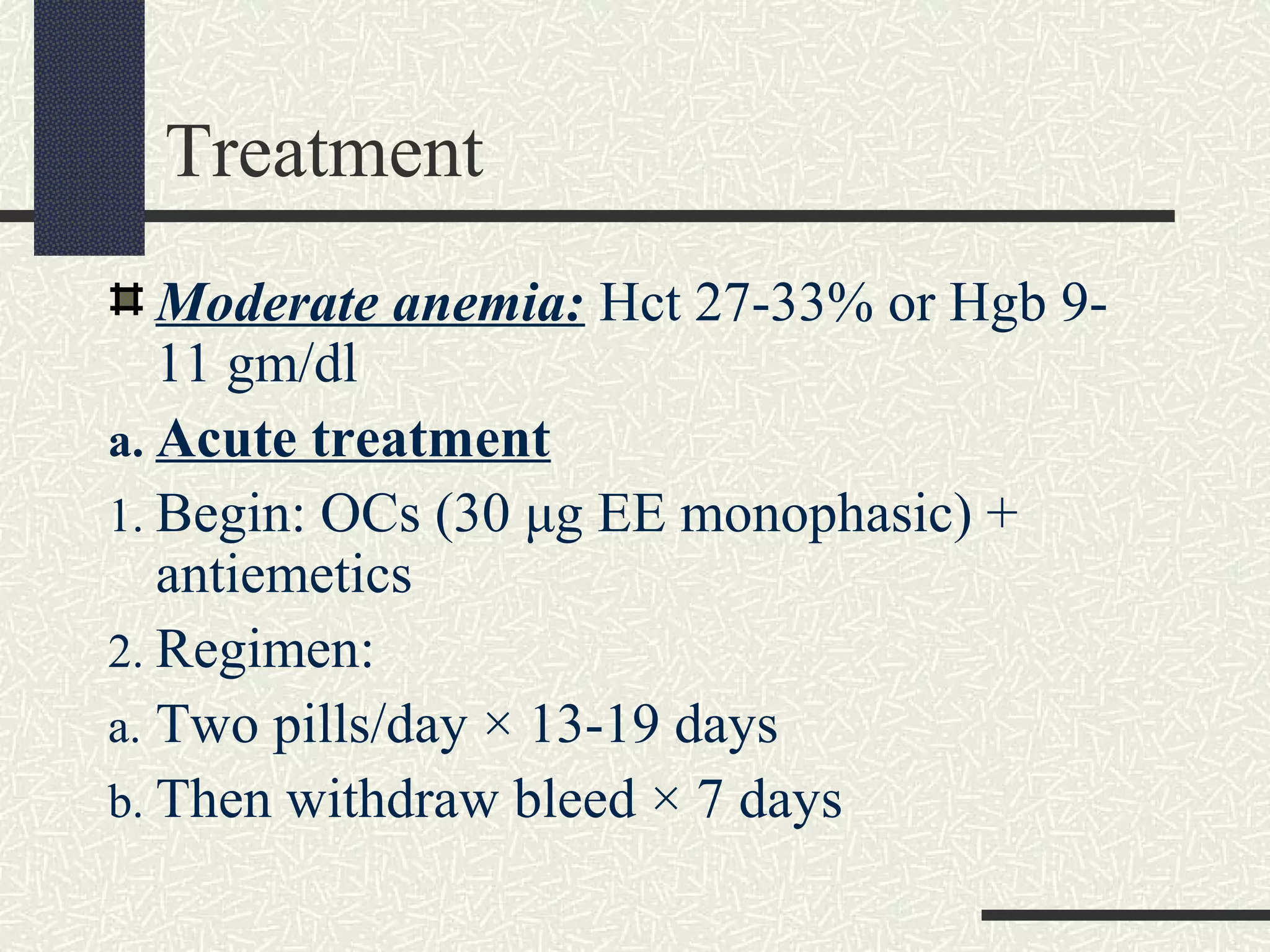
This document discusses variations in the menstrual cycle, including causes and treatments. It defines normal menstrual cycles and various types of irregularities including variations in frequency, amount, and duration. Common causes of irregularities include stress, excessive exercise, medications, medical conditions, and endocrine disorders. Dysfunctional uterine bleeding is described as abnormal bleeding without organic disease, often due to anovulation. Treatment depends on severity of anemia and may include oral contraceptives, iron supplementation, or blood transfusion in severe cases.