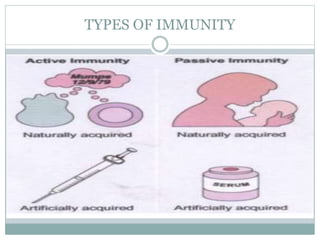
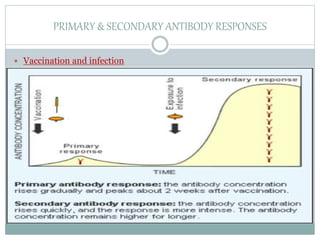
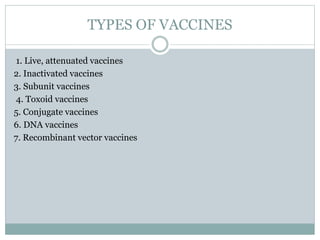
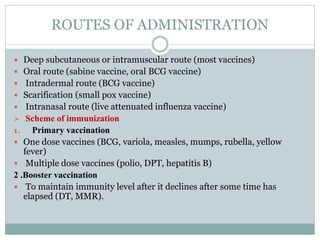
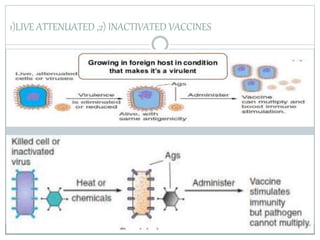
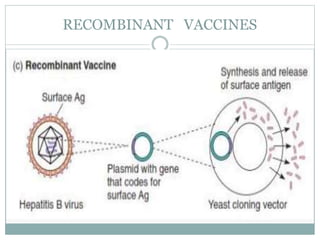
Vaccines are biological preparations that improve immunity to particular diseases. They contain agents that resemble disease-causing microorganisms and stimulate the immune system to recognize and destroy them. Edward Jenner developed the smallpox vaccine in 1796 by inoculating a boy with cowpox to produce immunity to smallpox. There are several types of vaccines including live attenuated, inactivated, subunit, toxoid, conjugate, DNA, and recombinant vector vaccines. Vaccines are administered through various routes and provide both primary and secondary immune responses. They have played a crucial role in reducing disease burden globally.