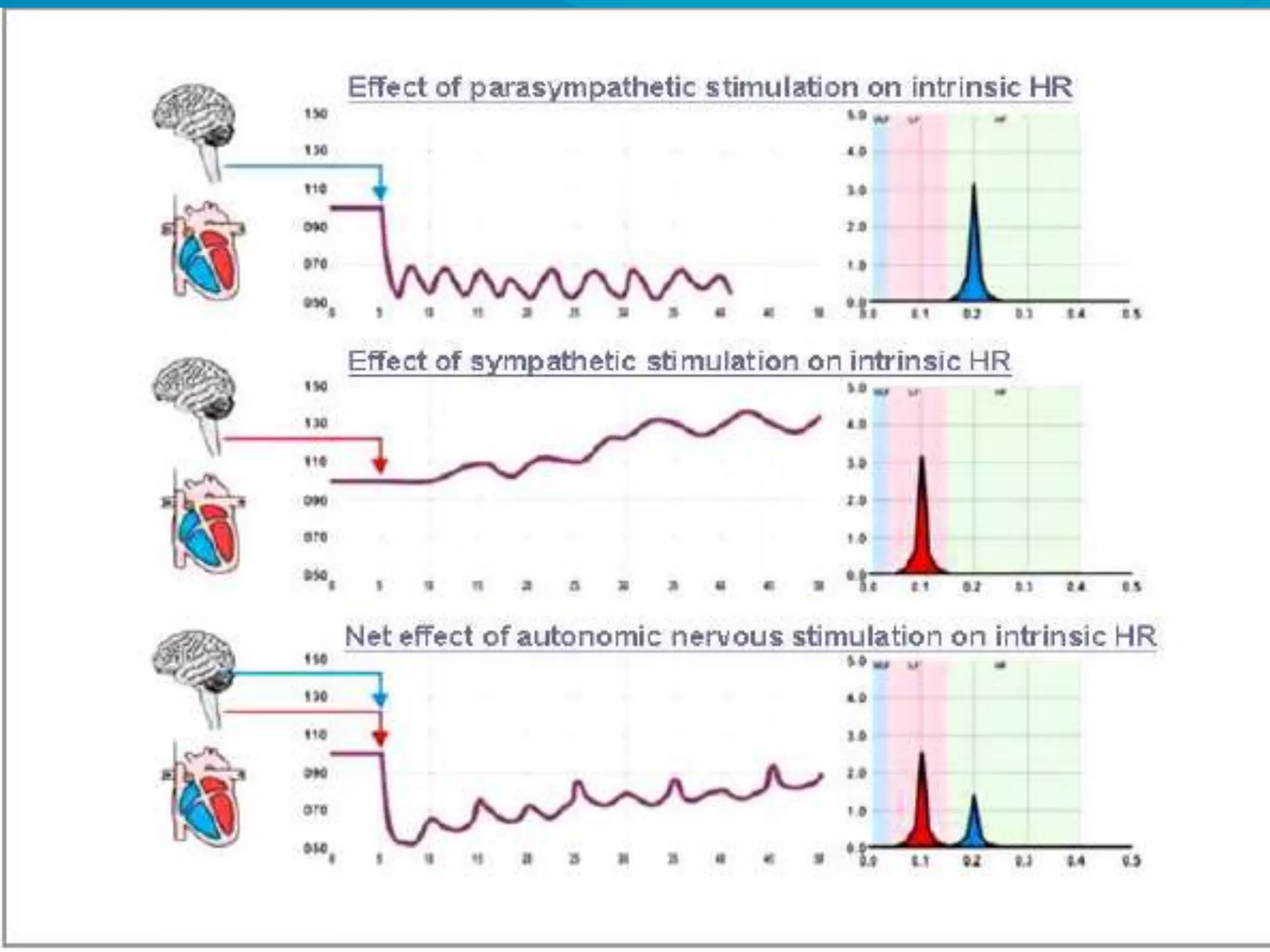
Syncope is a transient loss of consciousness with spontaneous recovery, commonly seen in emergency settings. Despite advancements, diagnosing its etiology remains challenging and often involves inadequate testing. The tilt table test is highlighted as a crucial diagnostic tool for unexplained syncope, particularly for patients suspected of vasovagal syncope.