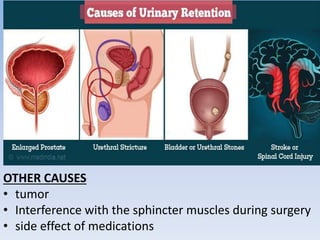
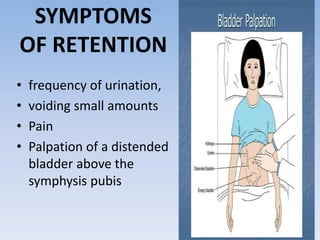
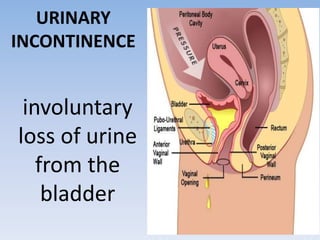
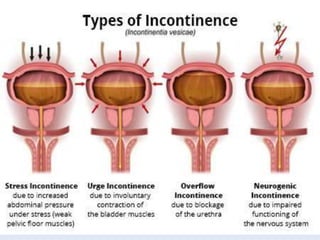
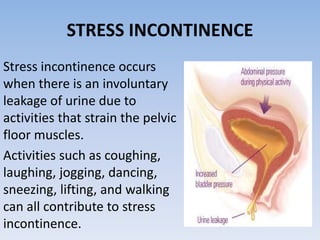
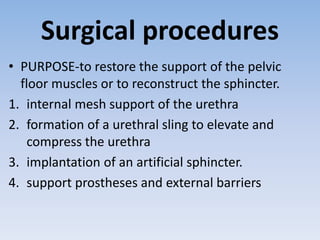
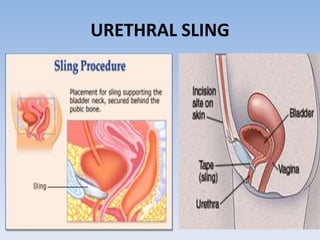
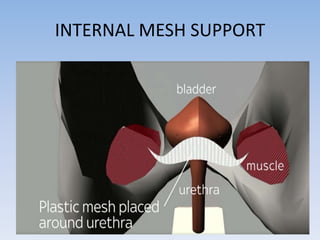
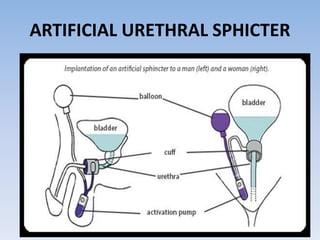
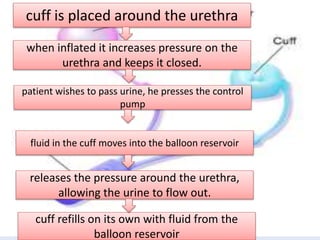
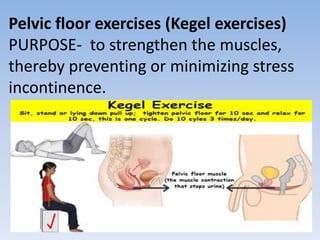
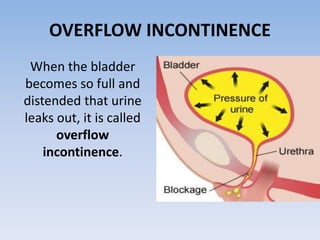
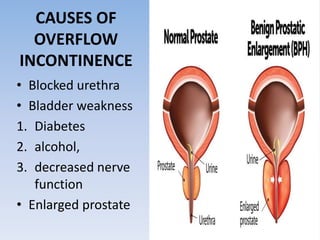
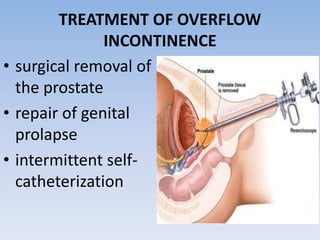
The document outlines urinary retention and incontinence, detailing their symptoms, causes, diagnosis, and treatment options. Urinary retention is characterized by the inability to void despite the urge, with causes such as tumors and medication side effects, while incontinence can be classified into types including stress and urge incontinence, each with specific management strategies. Treatments include medications, surgical interventions, pelvic floor exercises, and lifestyle modifications to improve bladder control.