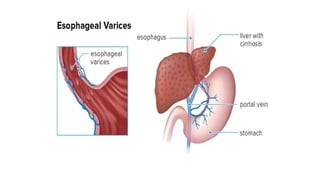
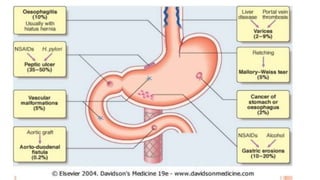
1. Upper gastrointestinal bleeding is a medical emergency caused by bleeding in the upper digestive tract proximal to the duodenojejunal junction. Common causes include esophageal varices, peptic ulcers, and Mallory-Weiss tears.
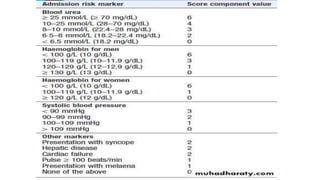
2. Symptoms include hematemesis (vomiting of blood) and melena (black tarry stools), and clinical assessment focuses on signs of blood loss severity. The Modified Blatchford Score stratifies bleeding risk.
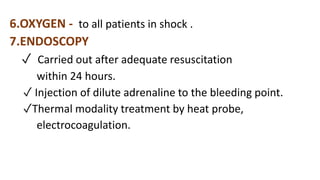
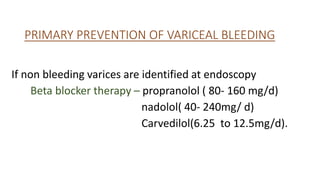
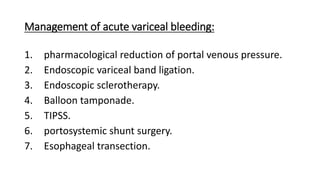
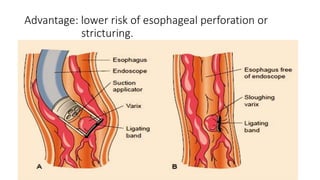
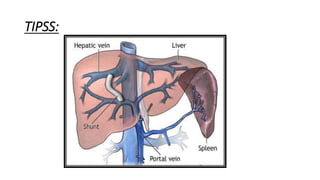
3. Initial management involves intravenous access, fluid resuscitation, gastric lavage, medications, and urgent endoscopy for diagnosis and treatment such as injection therapy or band ligation. Surgery or TIPSS procedure may be needed for