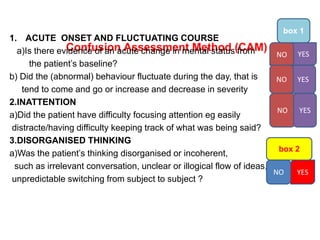
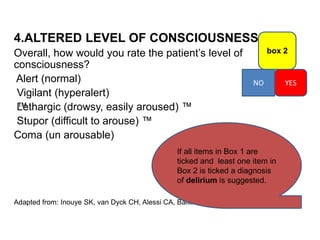
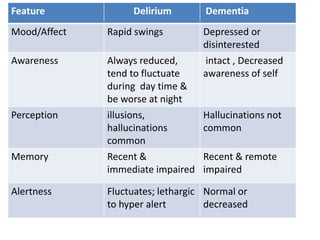
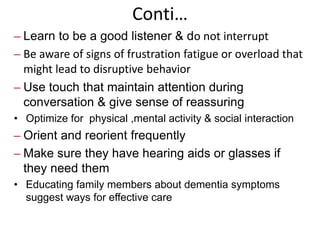
The document discusses the differences between delirium and dementia. Delirium is characterized by acute onset, fluctuating symptoms, and altered consciousness. It is often caused by medical conditions or medications. Dementia is a progressive decline in cognitive functions caused by conditions like Alzheimer's disease. It has a gradual onset and stable, non-fluctuating course. The document provides assessment tools for delirium and lists nursing interventions to manage symptoms and create a therapeutic environment for elderly patients with these conditions.