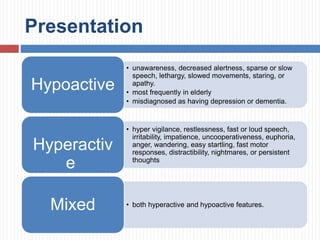
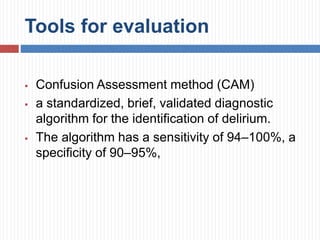
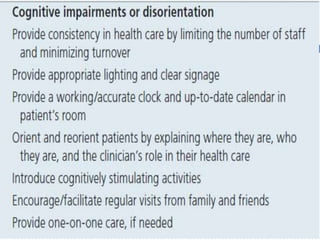
An 83-year-old woman presented with fever, shortness of breath, and poor oral intake. She has a history of multiple medical conditions and is on several medications. On examination, she has a fever and signs of respiratory distress. The physician is concerned about pneumonia and increased depression, but her cognitive status was not assessed. Delirium is an acute fluctuating syndrome of altered attention, awareness and cognition, especially common in elderly hospitalized patients. It is often misdiagnosed as depression or dementia. Non-pharmacological prevention and treatment of underlying causes are most important, while antipsychotics may be used short-term for severe symptoms if needed.