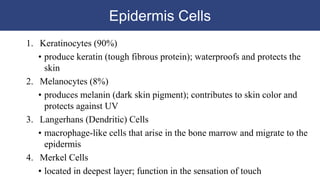
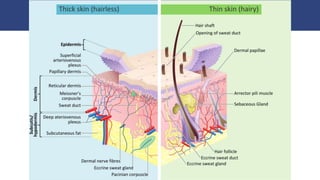
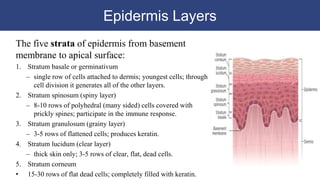
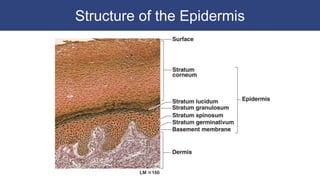
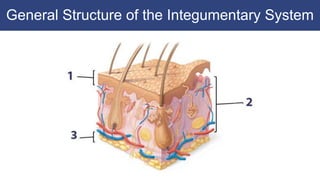
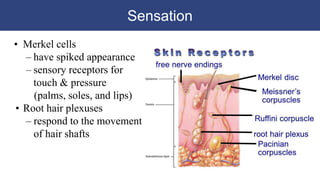
The epidermis is the outermost layer of skin and contains four main cell types: keratinocytes, melanocytes, Langerhans cells, and Merkel cells. Keratinocytes make up 90% of epidermal cells and produce keratin to protect the skin. Melanocytes produce melanin which contributes to skin color and protects against UV rays. The epidermis has multiple layers with keratinocytes forming the layers. The dermis lies below the epidermis and contains blood vessels, nerves, hair follicles, and glands. The hypodermis is made of adipose and connective tissue and stabilizes the skin. The skin helps regulate body temperature through sweating and blood vessel dilation and