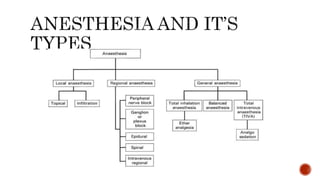
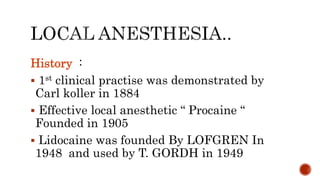
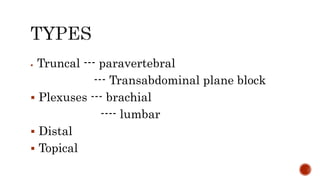
This document provides information on the history and types of local anesthesia. It discusses key details such as:
- Carl Koller demonstrated the first clinical use of local anesthesia in 1884 using procaine. Lidocaine was developed in 1948 and widely used.
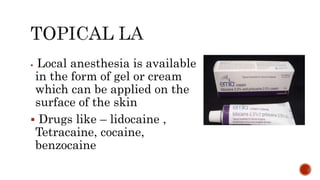
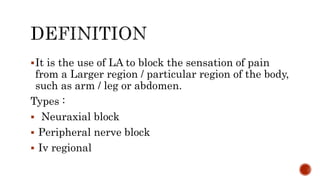
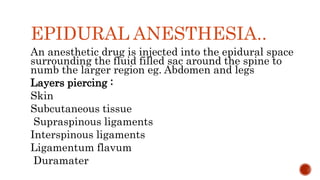
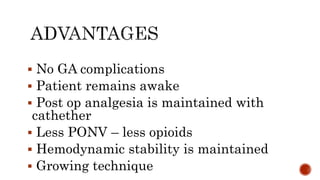
- Local anesthesia involves topical anesthetics or local infiltration of drugs like lidocaine to numb circumscribed body areas.
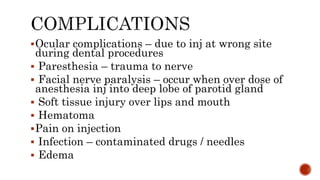
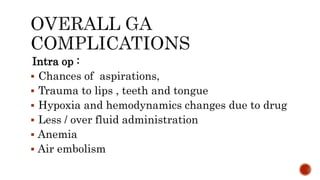
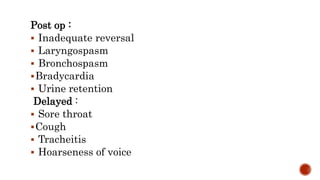
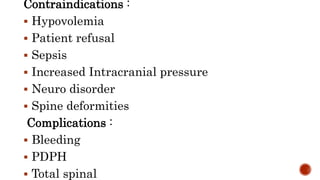
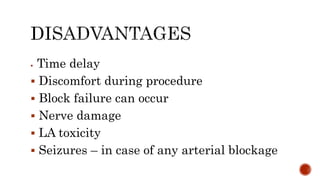
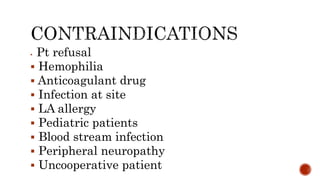
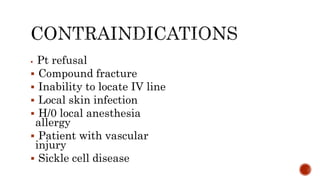
- Common uses are for excision procedures, dentistry work, dermatology procedures and biopsies. Potential risks include infection, hematoma, and nerve damage.