Anaesthesia
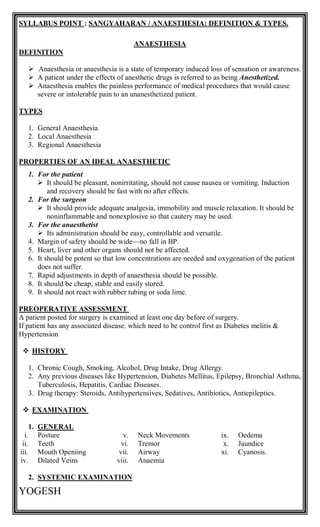
- 1. YOGESH SYLLABUS POINT : SANGYAHARAN / ANAESTHESIA: DEFINITION & TYPES. ANAESTHESIA DEFINITION Anaesthesia or anaesthesia is a state of temporary induced loss of sensation or awareness. A patient under the effects of anesthetic drugs is referred to as being Anesthetized. Anaesthesia enables the painless performance of medical procedures that would cause severe or intolerable pain to an unanesthetized patient. TYPES 1. General Anaesthesia 2. Local Anaesthesia 3. Regional Anaesthesia PROPERTIES OF AN IDEAL ANAESTHETIC 1. For the patient It should be pleasant, nonirritating, should not cause nausea or vomiting. Induction and recovery should be fast with no after effects. 2. For the surgeon It should provide adequate analgesia, immobility and muscle relaxation. It should be noninflammable and nonexplosive so that cautery may be used. 3. For the anaesthetist Its administration should be easy, controllable and versatile. 4. Margin of safety should be wide—no fall in BP. 5. Heart, liver and other organs should not be affected. 6. It should be potent so that low concentrations are needed and oxygenation of the patient does not suffer. 7. Rapid adjustments in depth of anaesthesia should be possible. 8. It should be cheap, stable and easily stored. 9. It should not react with rubber tubing or soda lime. PREOPERATIVE ASSESSMENT A patient posted for surgery is examined at least one day before of surgery. If patient has any associated disease. which need to be control first as Diabetes melitis & Hypertension HISTORY 1. Chronic Cough, Smoking, Alcohol, Drug Intake, Drug Allergy. 2. Any previous diseases like Hypertension, Diabetes Mellitus, Epilepsy, Bronchial Asthma, Tuberculosis, Hepatitis, Cardiac Diseases. 3. Drug therapy: Steroids, Antihypertensives, Sedatives, Antibiotics, Antiepileptics. EXAMINATION 1. GENERAL i. Posture ii. Teeth iii. Mouth Openiing iv. Dilated Veins v. Neck Movements vi. Tremor vii. Airway viii. Anaemia ix. Oedema x. Jaundice xi. Cyanosis. 2. SYSTEMIC EXAMINATION
- 2. YOGESH SYSTEM EXAMINATION 1. Respiratory System Asthma, Tuberculosis, Emphysema, COPD 2. Airway Mouth opening, Temporomandibular Joint Assessment 3. CVS HTN, IHD, Arrhythmias, Cardiac Failure, Valvular Diseases 4. Spine Curvature, Intervertebral Space, Skin over the area for any infn . 5. Other Systems Abdomen, Skeletal System PREOPERATIVE INVESTIGATIONS 1. Haematocrit 2. Blood Sugar 3. Blood Urea 4. Serum Creatinine 5. Electrolytes 6. Chest X-Ray 7. Blood-Gas Analysis 8. Cardiac Assessment 9. Renal Function Tests 10.Liver Function Tests 11.ECG PRE OPERATIVE PREPARATION 1. Establish a good conversation with patient. 2. Collect History of patient with examination. 3. Informed written consent should be taken. 4. If significant disease is present, then first it is brought under controlled. 5. Strictly NBM before 4 hrs of surgery. 6. Control of respiratory and cardiac diseases. 7. Improvement of Hb% status, if anaemia is present. 8. Preoperative antibiotics are given. 9. Blood should be kept ready for major cases. 10.Starvation for 4 hours for liquids and 6 hours for solids. 11.Bladder and bowel should be emptied to prevent soiling on the operation table. 12.Urinary catheter may be passed and enema may 13.Dentures, contact lenses, jewellery must be removed. 14.Surgical area should be cleaned and properly prepared. PREOPERATIVE MEDICATIONS CAUSE DRUGS USED DOSE To reduce Sedation and Anxiety Pethidine Morphine & Diazepam 50 mg 10 mg To reduce Vomiting Promethazine 12.5 mg To reduce Secretion Inj. Atropine 0.6 mg Blood Loss Blood Transfusion If Needed PHYSICAL EXAMINATION 1. Oral Hygiene 2. Examination of loose & artificial teeth 3. Nutritional & Hydration Status 4. Body Built 5. Pallor 6. Clubbing & Cyanosis 7. BP 8. Heart Sounds 9. Peripheral Pulsation EQUIPMENTS FOR ANAESTHESIA 1. Laryngeal scope 2. Endo Tracheal Tube (ETT) 3. Oropharyngeal airway 4. Nasopharyngeal airway 5. Ambubag 6. Boyle’s apparatus 7. Pulse oximeter 8. Cardiac monitor
- 3. YOGESH 9. B. P. Instrument 10.Stethoscope 11.Spinal Needle 12.Emergency drug Tray 13.Suction catheter 14.Source of 02 CLASSIFICATION (ACC. TO AMERICAN SOCIETY OF ANESTHESIOLOGISTS (ASA) ) GRADE FEATURE ASA I No abnormality ASA II Mild systemic disorders ASA III Moderate systemic disease with normal activity ASA IV Severe systemic disease that is threatening to the life of the patient ASA V Moribunt- not expected to survive 24 hrs with or without operation. Patient is dead posted for organ donation. I. LOCAL ANAESTHESIA – DRUGS, TECHNIQUES, INDICATIONS, CONTRAINDICATIONS, COMPLICATIONS AND THEIR MANAGEMENT. DEFINITION LA is defined as reversible depression of nerve impulse conduction leading to temporary loss of sensation and relief of pain because of disturbed nerve conductivity. Local anaesthesia is any technique to induce the absence of sensation in a specific part of the body, generally for the aim of inducing local analgesia, that is, local insensitivity to pain, although other local senses may be affected as well. Local anaesthesia is anaesthesia of a small part of the body such as a tooth or an area of skin. A local anaesthetic is a medication that causes reversible absence of pain sensation, although other senses are often affected, as well. It blocks both conduction and generation of impulse. CLASSIFICATION : 1. Injectable Anaesthetics A. Low Potency, Short Duration Procaine Chloroprocaine B. Intermediate Potency And Duration Lidocaine (Lignocaine) Prilocaine C. High Potency, Long Duration Tetracaine (Amethocaine) Bupivacaine Ropivacaine Dibucaine (Cinchocaine ) 2. Surface Anaesthetics A. Soluble Cocaine Lidocaine Tetracaine Benoxinate B. Insoluble Benzocaine Oxethazaine Butylaminobenzoate TECHNIQUES & USES
- 4. YOGESH 1. SURFACE ANAESTHESIA / TOPICAL ANAESTHESIA Skin is anaesthetized by local anaesthetic agents used as spray, ointment, cream, jelly and lotion. 2. INFILTRATION ANAESTHESIA Injection of local anesthetic drug into area which is to be incised in a circular manner. Infiltration is used for minor operations, e.g. incisions, excisions, hydrocele, herniorrhaphy, etc. when the area to be anaesthetised is small. 3. FIELD BLOCK It is produced by injecting the LA subcutaneously which blocks entire field of excisionwhere disease is located. 4. NERVE BLOCK It is produced by injecting the LA around the appropriate nerve trunks or plexuses. Frequently performed nerve blocks are—lingual, intercostal, ulnar, sciatic, femoral, brachial plexus, trigeminal, facial, phrenic, etc.—used for tooth extraction, operations on eye, limbs, abdominal wall, fracture setting, trauma to ribs, neuralgias, persistent hiccup, etc. The primary purpose of nerve block anaesthesia is to abolish pain and other sensations. TECHNIQUE Supraclavicular approach is commonly used Needle is passed downwards, backwards and medially towards first rib, 1cm above midpoint of clavicle Once needle hits the first rib, 15-20 ml of 1.5% xylocaine is injected .
- 5. YOGESH 5. INTRAVENOUS LOCAL ANAESTHESIA ( BIER’S BLOCK ) TECHNIQUE Limb is exsanguinated & occluded with tourniquet with pressure 30mmhg more than systolic pressure of the patient. Needle is placed in the selected vein. Xylocaine – 40 ml of 0.5% for upper limb 80ml of 0.25% for lower limb Side effects: Hypotension, Convulsions, Death 6. SPINAL ANAESTHESIA Spinal anaesthesia is also known as saddle block/saddle anaesthesia . It is the injection of LA into the subarachnoid space between L2–3 or L3–4 i.e. below the lower end of spinal cord, causing loss of sympathetic tone, sensation and motor function. Spinal anaesthesia is used for operations on the lower limbs, pelvis, lower abdomen, e.g. prostatectomy, fracture setting, obstetric procedures, caesarean section, etc When they are injected in sub arachnoid space it is called as Spinal Anaesthesia. Saddle Anaesthesia means after injecting anesthetic drug in subarachnoid space patient gives sitting position on table for 10 min. Then it is known as Saddle Block or Saddle Anaesthesia. TYPES TYPE INJ. LEVEL 1. Caudal Anaesthesia Upto L5 2. Low Spinal Anaesthesia Upto L1 3. Mid Spinal Anaesthesia Upto T10 4. High Spinal Anaesthesia Upto T6 5. Unilateral Spinal Anaesthesia USEFUL DRUGS IN SPINAL ANAESTHESIA ADVANTAGES 1. Profound relaxation. 2. Retention of consciousness. 3. No irritation of lungs 4. Operative hemorrhage less due to fall of Blood Pressure 5. Economical DISADVANTAGES
- 6. YOGESH 1. Technical difficulties by unexpert. 2. CSF leak INDICATIONS 1. Provide excellent muscle relaxation 2. Prostectomy 3. LSCS 4. Hysterectomy and Hemorrhoidectomy 5. Fistulectomy 6. Lower limb fractures, 7. Urological, gynaecological, lower limb, & below umbilical operations. 8. Respiratory diseases. 9. Suffering from liver & kidney diseases as well as diabetes. CONTRAINDICATIONS 1. Without patient’s will 2. Shock 3. Hypoxia 4. Severe anemia 5. Dehydration 6. Active neurological disease 7. Infection 8. Hypotension and hypovolemia. 9. Uncooperative or mentally ill patients. 10.Infants and children—control of level is difficult. 11.Bleeding diathesis. 12.Raised intracranial pressure. 13.Vertebral abnormalities e.g. kyphosis, lordosis, etc. 14.Sepsis at injection site. PROCEDURE OF SPINAL ANAESTHESIA 1. Spinal Anaesthesia may be administrated to patient in sitting position or in right & left lateral position. 2. The patient lies either in left or right lateral position & back is kept parallel to edge of table. 3. Leg should be flexed while in sitting position patient sits on table with back bent forward & advised to rest his arm on his shoulde. 4. The back is cleaned with savlon, iodine & spirit, under strict aseptic precautions. 5. Vertebral spines are identified from highest point of iliac crest L3, L4. intervertebral space L 4 & L5 space commonly used. 6. In uncooperative patients, wheel of local anesthetic drug is injected at the site of spinal anaesthesia. 7. Lumbar puncture needle 25 to 27 G is inserted in midline. between intervertebral space perpendiculars to skin. 8. Spinal needle passes following structures. . i. Skin ii. Subcutaneous tissue iii. Supra spinal ligament iv. Inter spinal ligament v. Ligamentum Flaveum vi. Epidural space vii. Dura. matter viii. Sub arachnoid space
- 7. YOGESH 9. Correct position of tip of needle is identified by:- a. Free resistant to hand b. Continuous CSF free flow 10.After making confirmation tip of needle is in subarachnoid space. Drug is then injected slowly as per requirement. COMPLICATIONS OF SPINAL ANAESTHESIA 1. Hypotension due to vasodilation 2. Septic meningitis 3. Paraplegia 4. Backachce 5. Cauda equina syndrome 6. Infection. 7. Retention of urine 8. Intravertebral disc injury 9. Headache 10.Respiratory depression CAUDAL ANAESTHESIA It is the sacral component of spidural space and access is through the sacral hiatus. PROCEDURE 1. It is given in lateral position. 2. Needle is inserted through the sacral hiatus to enter the caudal epidural space. 3. Drug is then injected into the space. INDICATIONS 1. Haemorrhoidal surgery 2. Circumcision 3. Small procedures in perineum like cystoscopy. COMPLICATIONS 1. Trauma to the anal canal 2. Intravascular injection 7. EPIDURAL ANAESTHESIA Epidural anaesthesia is a type of local anaesthesia. It isa direct block of spinal nerve roots in epidural space leading to centrifugal spread which affects the nerve in block known as epidural anaesthesia. TECHNIQUE 1. It can be done with the patient in the lateral decubitus position. 2. Epidural needle does not have sharp tip, so chance of puncture in dura matter is very rare. 3. In epidural anaesthesia 16 to 17 touhy needle is used. Needle is passed through the midline or para medium. Needle passes structure as similar to spinal anaesthesia except penetration into sub-arachnoid space. ADVANTAGES OF EPIDURAL ANAESTHESIA 1. It can be used for continuous repeated prolonged anaesthesia.
- 8. YOGESH 2. It can be used for postoperative analgesia. 3. It can be kept for several days. ADVANTAGES OF LOCAL ANAESTHESIA 1. Technically simpler. 2. GA is avoided. 3. Consciousness is retained. 4. Pt. can have food earlier after surgery. COMPLICATIONS OF LOCAL ANAESTHESIA 1. CNS effects are - i. Light-Headedness ii. Dizziness iii. Auditory And Visual Disturbances iv. Mental Confusion v. Disorientation vi. Shivering vii. Twitching viii. Involuntary Movements ix. Finally Convulsions x. Respiratory Arrest. These can be prevented and treated by diazepam. 2. Cardiovascular toxicity of LAs – i. Bradycardia ii. Hypotension iii. Cardiac Arrhythmias iv. Vascular Collapse 3. Injection of LAs may be painful. 4. Delayed wound healing . 5. Hypersensitivity reactions- i. Rashes ii. Angioedema iii. Dermatitis iv. Contact Sensitization v. Asthma vi. Rarely Anaphylaxis Occur. CONTRAINDICATION TO LOCAL ANAESTHESIA Absolute Contraindications 1. History of Allergy to Local Anesthetic Agents 2. Local anesthetic agents belonging to the same chemical group should not be used. 3. Documented Allergy to Other Constituents of the solution. 4. History of allergy to any of the constituents of the local anesthetic solution. Relative Contraindications 1. Fear and apprehension 2. Presence of acute inflammation or Suppurative infection at the site of insertion of the needle. 3. Infants or small children 4. Mentally retarded patients 5. Restricted mouth opening 6. Patients with Medical disease- i. Cardiovascular Disease ii. Hepatic Dysfunction iii. Renal Dysfunction iv. Clinical Hyperthyroidism DIFFERENCE BETWEEN SPINAL AND EPIDURAL ANAESTHESIA
- 9. YOGESH SPINAL ANAESTHESIA EPIDURAL ANAESTHESIA 1. Onset of blockage is fast ( 1 min.). 2. Only lumbar puncture. 3. Duration limited. 4. Needle used : 23-25 no. 5. Less chance of CSF contamination. 6. Small dose inj. 7. Headache absent. 8. Backache more persistant. 9. Less severe hypotension. 10.Faulty anaesthesia. 1. Onset of blockage is slow ( 2 min.). 2. Lumbar, sacral, thoracic, cervical puncture. 3. Duration prolonged. 4. Needle used : 16-17 no. 5. More chance of CSF contamination. 6. Large dose inj. 7. Headache present. 8. Backache present. 9. More severe hypotension. 10.Excellent anaesthesia. I. REGIONAL AND GENERAL ANAESTHESIA – DRUGS, TECHNIQUES, INDICATIONS, CONTRAINDICATIONS, COMPLICATIONS AND THEIR MANAGEMENT. REGIONAL ANAESTHESIA DEFINITION Regional anaesthesia is the use of local anesthetics to block sensations of pain from a large area of the body, such as an arm or leg or the abdomen by using local anaesthetic agent. Regional anaesthesia allows a procedure to be done on a region of the body without your being unconscious. For regional anaesthesia, the anesthetic is injected close to a nerve, a bundle of nerves, or the spinal cord. DRUGS USES Regional anaesthesia is most often used when the procedure: Is confined to a specific region of the body.
- 10. YOGESH Involves a large area of the body where injection of large amounts of an anesthetic might cause side effects that affect the entire body. Does not require general anaesthesia. RISKS AND COMPLICATIONS FROM REGIONAL ANAESTHESIA 1. For regional anaesthesia, an anesthetic is injected close to a nerve, a bundle of nerves, or the spinal cord. In rare cases, nerve damage can cause persistent numbness, weakness, or pain. 2. Regional anaesthesia also carries the risk of systemic toxicity if the anesthetic is absorbed through the bloodstream into the body. 3. Other complications include heart or lung problems, and infection, swelling, or bruising (hematoma) at the injection site. CONTRAINDICATIONS DIFFERENCE BETWEEN LOCAL ANAESTHESIA & REGIONAL ANAESTHESIA LOCAL ANAESTHESIA REGIONAL ANAESTHESIA 1. A local anaesthesia only blocks the injected direct area. 2. Agents such as lidocaine or marcaine are local anesthetics that can be injected directly into the area to be operated upon with a 1-4 hour blockade. 3. Local anaesthesia numbs just a small area of tissue where a minor procedure is to be done. 4. Local anaesthesia is where a drug is injected near nerves in or through the skin providing loss of sensation to the area of the surgical operation. 5. Risks include infection, 1. Regional anaesthesia blocks pain to a large portion of the body at one time. 2. This includes epidural, spinal, and peripheral nerve blocks. The nerve block is delivered approximate to the nerve bundle or group for peripheral nerve blockade. 3. Regional anaesthesia numbs a larger (but still limited) part of the body and does not make the person unconscious. 4. Regional anaesthesia is where a drug is injected into the veins of an arm or leg while using a tourniquet to create temporary loss of feeling and/or movement of a limb. 5. Risks include infection, convulsions,
- 11. YOGESH convulsions, weakness, persistent numbness, residual pain and injury to the blood vessels. 6. For local anaesthesia the patient is conscious. persistent numbness, residual pain and injury to the blood vessels. 6. For regionals, the patient can either be under conscious sedation or awake. GENERAL ANAESTHESIA DEFINITION General anaesthetics (GAs) are drugs which bring about loss of modalities of sensation particularly pain along with all reversible loss of all sensation. The cardinal features of general anaesthesia are: 1. Loss of all sensation, especially pain 2. Sleep (unconsciousness) and amnesia 3. Immobility and muscle relaxation 4. Abolition of somatic and autonomic reflexes. CLASSIFICATION MECHANISM OF ACTION
- 12. YOGESH Depresses all functional unit of CNS. Particularly inhibit ascending reticular artibating system ( ARAS) which maintain state of wakefulness. STAGES OF ANAESTHESIA 1. STAGE OF ANALGESIA Starts from beginning of anaesthetic inhalation and lasts upto the loss of consciousness. Pain is progressively abolished. Patient remains conscious, can hear and see, and feels a dream like state; amnesia develops by the end of this stage. Reflexes and respiration remain normal. Though some minor operations can be carried out during this stage, it is rather difficult to maintain—use is limited to short procedures. 2. STAGE OF DELIRIUM From loss of consciousness to beginning of regular respiration. Apparent excitement is seen—patient may shout, struggle and hold his breath; muscle tone increases, jaws are tightly closed, breathing is jerky; vomiting, involuntary micturition or defecation may occur. Heart rate and BP may rise and pupils dilate due to sympathetic stimulation. No stimulus should be applied or operative procedure carried out during this stage. This stage is inconspicuous in modern anaesthesia. 3. SURGICAL ANAESTHESIA Extends from onset of regular respiration to cessation of spontaneous breathing. This has been divided into 4 planes which may be distinguished as: i. PLANE 1 - Roving eyeballs. This plane ends when eyes become fixed. ii. PLANE 2 - Loss of corneal and laryngeal reflexes. iii. PLANE 3 - Pupil starts dilating and light reflex is lost. iv. PLANE 4 - Intercostal paralysis, shallow abdominal respiration, dilated pupil. As anaesthesia passes to deeper planes, progressively— muscle tone decreases, BP falls, HR increases with weak pulse, respiration decreases in depth and later in frequency also. 4. MEDULLARY PARALYSIS
- 13. YOGESH Cessation of breathing to failure of circulation and death. Pupil is widely dilated, muscles are totally flabby, pulse is thready or imperceptible and BP is very low. INHALATIONAL ANAESTHETICS TECHNIQUES OF INHALATION OF ANAESTHETICS 1. Open Drop Method Liquid anaesthetic is poured over a mask with gauze and its vapour is inhaled with air. Eg. Ether. 2. Through Anaesthetic Machines The gases are delivered to the patient through a tightly fitting face mask or Endotracheal Tube or Boyle’s Apparatus. Eg. Nitrous oxide, Ethylene. INHALATIONAL ANAESTHETICS DRUGS DEFINITION ADVANTAGES DISADVANTAGES 1. Nitrous oxide Non-Irritating Better Smelling Colorless Inorganic Gas Safest Anesthetic Drug Non- Inflammable Non-irritant to patient Pleasant to inhale Post - operative complication is less Muscle relaxation is unsatisfactory Teratogenic effect Blood pressure is increased 2. Ether Colorless, Volatile Liquid Used for all types of surgery Safe Simple to administrate Little toxic axn. on heart Highly irritative to upper respiratory tract Vapor inhalation is unpleasant for patient Increases secretions of all the glands 3. Halothane (Fluothane) Colorless Liquid Volatile Anesthetic Volatile anesthetic drug & most expensive. Non - inflammable Non-irritant to respiratory tract. Rapid,smooth & with fast recovery Respiratory Depression No Analgesic Properties Hepatotoxic Effect INTRAVENOUS ANAESTHETICS
- 14. YOGESH DRUGS DEFINITION ADVANTAGES DISADVANTAGES 1. Thiopentone Sodium Ultra short acting barbiturate. Used mainly for minor surgeries. Non-irritant to lungs & non-explosrve. Less nausea & vomiting. Muscle relaxation is rapid. Fall in blood pressure. Poor analgesic & relatively large quantity is needed to produce true anaesthesia. Recovery period is long & drowsiness persists after one hour. 2. Ketamine Also known, as “Dissociative (sudden temporary alteration) anaesthesia. Respiration is not depressed. Muscle tone increases. Useful for burn dressing & I & D. Good for repeated use. Dangerous for IHD patients. Delirium, Hallucinations & Involuntary movements. Heart rate, cardiac output & blood pressure are elevated. COMPLICATIONS OF GENERAL ANAESTHESIA 1. Hypotension 2. Respiratory Depression 3. Laryngeal Spasm 4. Delirium 5. Nausea 6. Vomiting 7. Organ Toxicity 8. Airway Obstruction 9. Bronchospasm 10.Respiratory Failure 11.Arrythmias 12.Cardiac Arrest 13.Renal Failure 14.Hepatic Failure
- 15. YOGESH