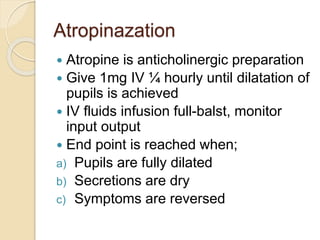
The document discusses principles of first aid and emergency care for trauma patients, including assessing and managing the ABCs (airway, breathing, circulation). It covers common emergencies like asphyxia, wounds, shock, and their signs, causes, and first aid treatments. The Heimlich maneuver and other airway management techniques like endotracheal intubation are described for establishing an open airway in emergency situations.