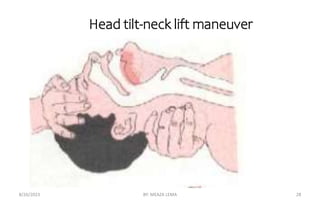
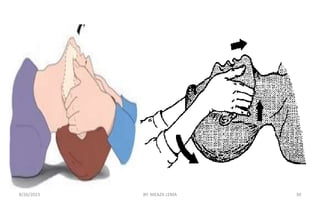
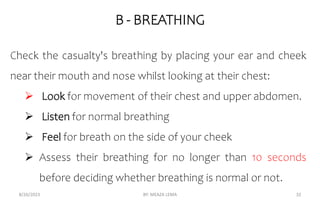
The document provides information on first aid and accident prevention. It defines first aid and outlines its importance, including preserving life, preventing further injury, and promoting healing. It also discusses general directions for providing first aid, such as assessing safety, identifying the problem, prioritizing patients, extricating victims, and arranging transportation. Additionally, it covers topics like the definition of important terms, reasons for giving first aid, values of training, and emergency patient assessment techniques.