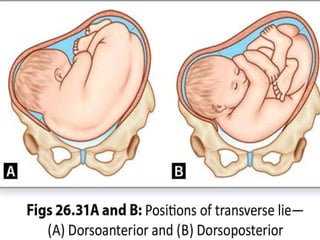
This document defines and discusses transverse lie, an abnormal fetal position where the long axis of the fetus is perpendicular to that of the mother. Key points include:
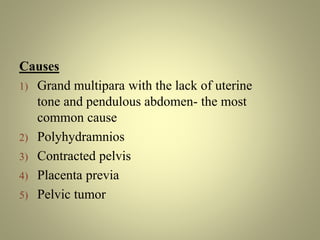
- Transverse lie results in a shoulder presentation and has a 1 in 200 incidence rate. It is more common in preterm/macerated fetuses and multiparous women.
- Diagnosis involves abdominal/pelvic examination and ultrasound to confirm the lie beyond 36 weeks.
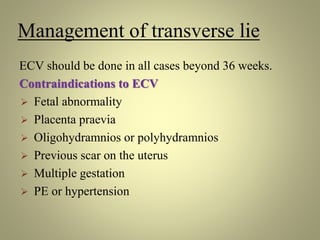
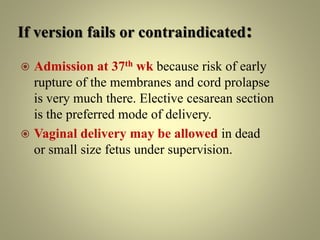
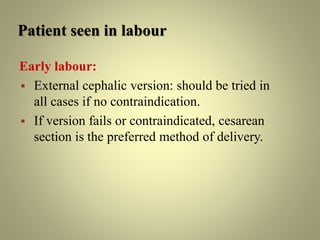
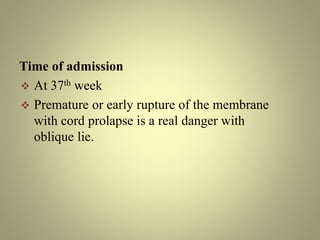
- Untreated transverse lie poses risks like cord prolapse and obstructed labor. Modern management includes external cephalic version or cesarean section for delivery.
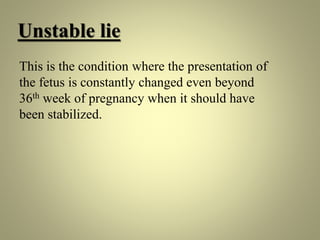
- Unstable lie with constantly changing presentation poses similar risks and is managed with version attempts and close monitoring