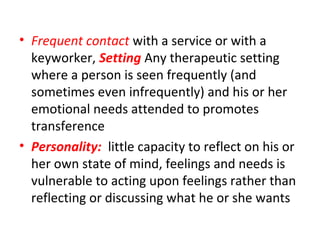
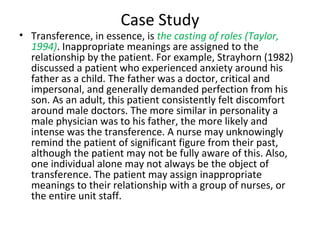
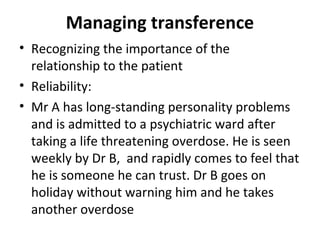
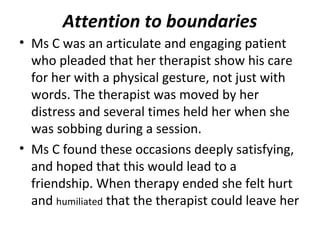
This document defines and discusses the concepts of transference and countertransference in mental healthcare. Transference refers to a client unconsciously transferring feelings and attitudes from past relationships onto their healthcare provider. Countertransference occurs when a provider transfers their own feelings onto a client. Recognizing transference and countertransference is important for providers to understand what is happening in the client relationship and avoid acting out. Managing these phenomena involves maintaining appropriate boundaries, being reliable, and using reflection and supervision to avoid reactive responses.