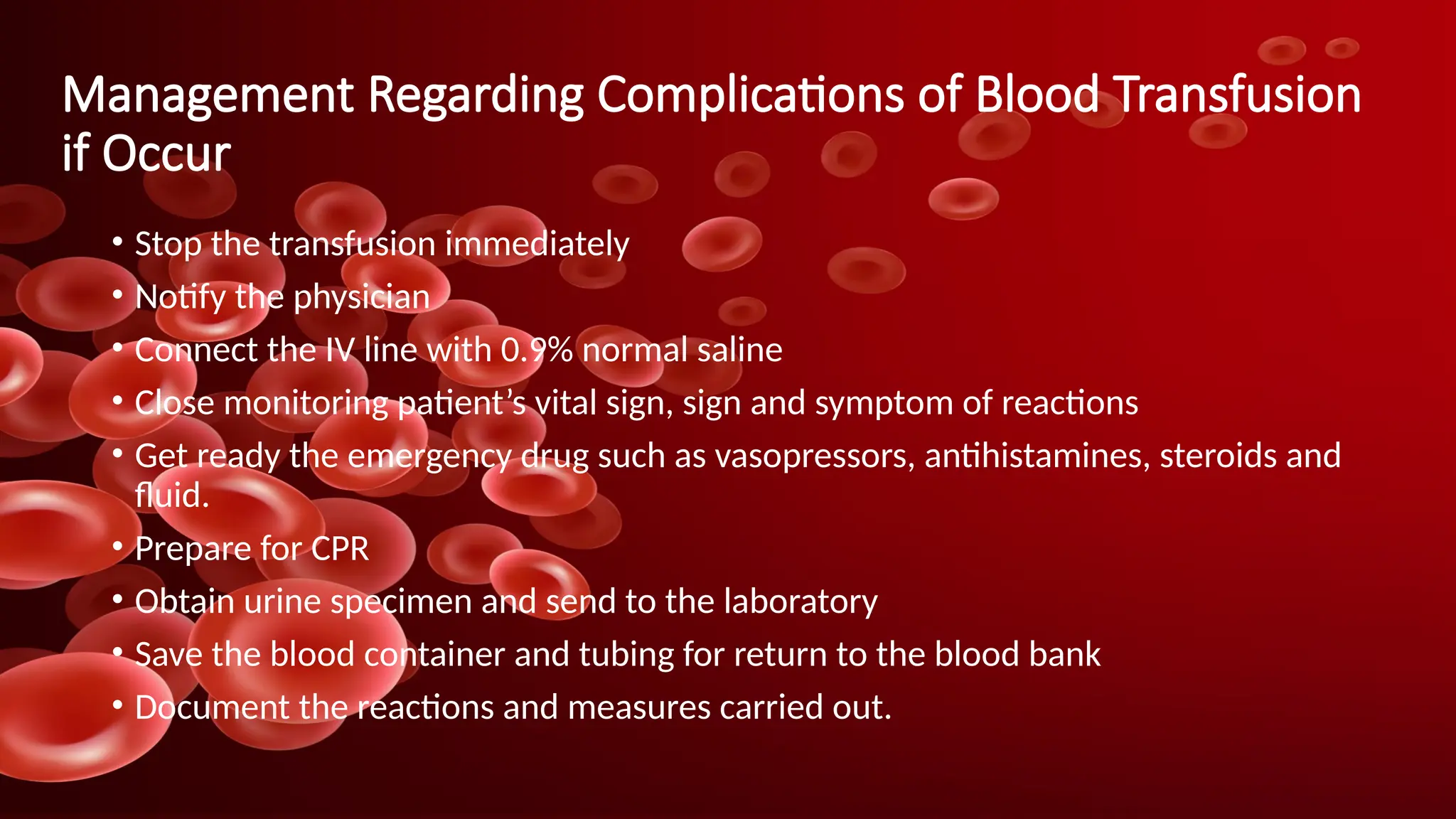
The document provides comprehensive information on blood transfusion, including its definition, indications, components, and the procedures for collection, storage, and administration. It outlines the types of blood transfusions, preparation instructions, and potential complications, including various transfusion reactions and their management. Emphasis is placed on the importance of compatibility in blood typing and the selection of healthy donors.