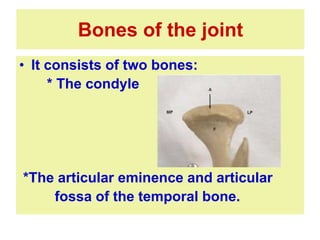
The temporomandibular joint (TMJ) is a complex synovial joint that connects the mandible to the temporal bone. It allows for hinge-like and gliding movements during functions like chewing and speaking. The TMJ is made up of the mandibular condyle, articular eminence of the temporal bone, an articular disc that divides the joint into two cavities, a joint capsule lined with synovial membrane, and ligaments. Various clinical conditions can affect the TMJ, including arthritis, injuries, dislocations, and myofascial pain dysfunction syndrome.