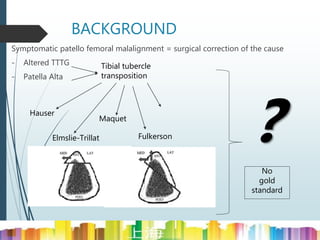
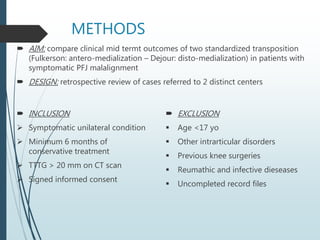
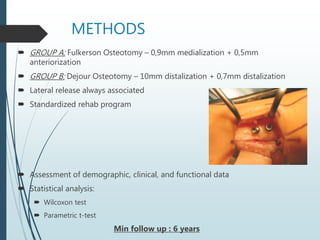
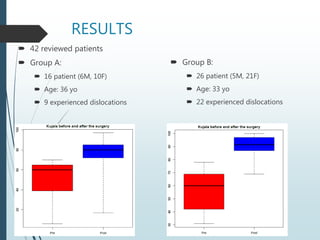
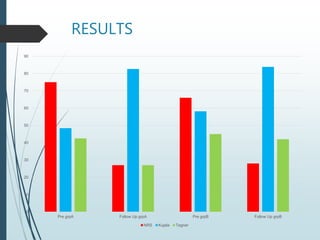
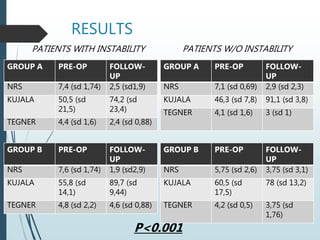
The document compares clinical outcomes of two tibial tubercle transposition techniques, anteromedialization (Fulkerson) and distomedialization (Dejour), in patients with symptomatic patellofemoral joint malalignment. It involved a retrospective review of 42 patients, with outcomes showing overlapping effectiveness between the two methods despite differences in surgical approaches. The findings indicate that while the procedures are effective, tailoring them to individual patient anatomy is crucial for optimal results.