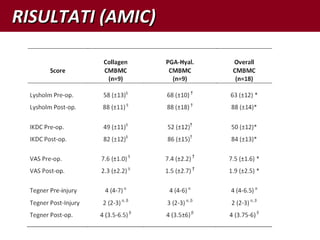
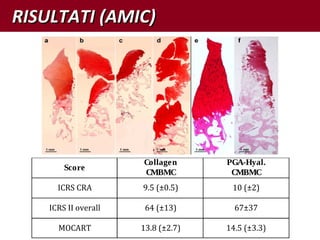
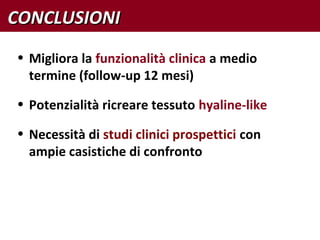
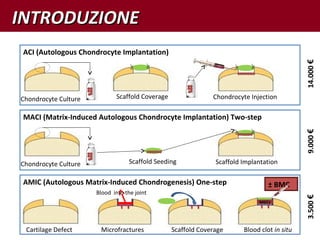
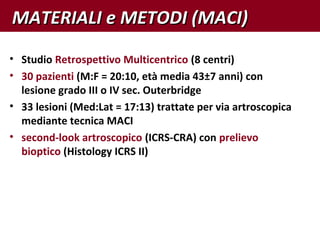
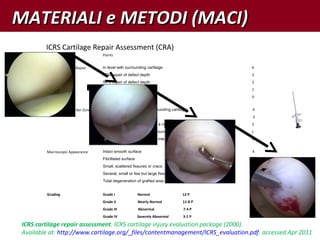
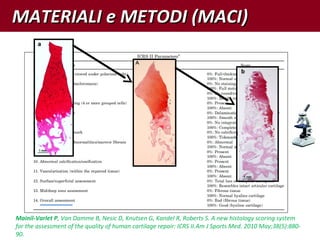
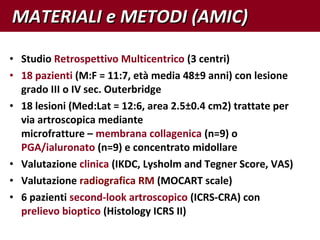
The document compares the results of MACI (matrix-induced autologous chondrocyte implantation), a two-step cartilage repair technique, to AMIC (autologous matrix-induced chondrogenesis), a one-step technique. A retrospective study of 30 patients who underwent MACI found mostly normal or near-normal arthroscopic and biopsy results. A separate study of 18 patients who received AMIC also found largely positive clinical outcomes and biopsy results indicating hyaline-like tissue, though further large prospective studies are still needed to directly compare the techniques.


![• Solo pochi studi in letteratura di sono focalizzati sulla
quantificazione dei risultati istologici dopo impianti ACI
Briggs TW, Mahroof S, David LA, Flannelly J, Pringle J, Bayliss M (2003) Histological evaluation of chondral defects after autologous
chondrocyte implantation of the knee. J Bone Joint Surg Br 85:1077-83
Brun P, Dickinson SC, Zavan B, Cortivo R, Hollander AP, Abatangelo G (2008) Characteristics of repair tissue in second-look and third-look
biopsies from patients treated with engineered cartilage: relationship to symptomatology and time after implantation. Arthritis Res
Ther 10:R132
Henderson I, Lavigne P, Valenzuela H, Oakes B (2007) Autologous chondrocyte implantation: superior biologic properties of hyaline cartilage
repairs. Clin Orthop Relat Res 455:253-61
Roberts S, McCall IW, Darby AJ, Menage J, Evans H, Harrison PE, Richardson JB (2003) Autologous chondrocyte implantation for cartilage
repair: monitoring its success by magnetic resonance imaging and histology. Arthritis Res Ther 5:R60-73
Roberts S, Menage J, Sandell LJ, Evans EH, Richardson JB (2009) Immunohistochemical study of collagen types I and II and procollagen IIA in
human cartilage repair tissue following autologous chondrocyte implantation. Knee 16:398-404
• Un solo studio ha analizzato biopsie di pazienti sottoposti a MACI
Zheng MH, Willers C, Kirilak L, Yates P, Xu J, Wood D, Shimmin A (2007) Matrix-induced autologous chondrocyte implantation (MACI): biological and
histological assessment. Tissue Eng 13:737-46
• Quasi niente si conosce dei risultati di tecniche One-step ± BMC
Giannini S, Buda R, Vannini F, Cavallo M, Grigolo B. One-step bone marrow-derived cell transplantation in talar osteochondral lesions. Clin
Orthop Relat Res 2009; 467:3307-20.
Saw KY, Anz A, Merican S, Tay YG, Ragavanaidu K, Jee CS, McGuire DA. Articular Cartilage Regeneration With Autologous Peripheral
Blood Progenitor Cells and Hyaluronic Acid After Arthroscopic Subchondral Drilling: A Report of 5 Cases With Histology.
Arthroscopy 2011 [Epub ahead of print]
INTRODUZIONEINTRODUZIONE](https://image.slidesharecdn.com/maciversusonestagesiot16-180118162713/85/Tecnica-MACI-versus-le-tecniche-one-step-4-320.jpg)




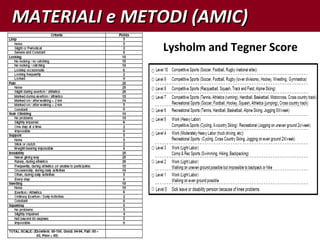
![MATERIALI e METODI (AMIC)MATERIALI e METODI (AMIC)nal of Radiology 57 (2006) 16–23
Table 2
Cartilage repair tissue grading scale (MOCART)
Variables
1. Degree of defect repair and filling of the defect
Complete (on a level with adjacent cartilage)
Hypertrophy (over the level of the adjacent cartilage)
Incomplete (under the level of the adjacent cartilage; underfilling)
>50% of the adjacent cartilage
<50% of the adjacent cartilage
Subchondral bone exposed (complete delamination or dislocation
and/or loose body)
2. Integration to border zone
Complete (complete integration with adjacent cartilage)
Incomplete (incomplete integration with adjacent cartilage)
Demarcating border visible (split-like)
Defect visible
<50% of the length of the repair tissue
>50% of the length of the repair tissue
3. Surface of the repair tissue
Surface intact (lamina splendens intact)
Surface damaged (fibrillations, fissures and ulcerations)
<50% of repair tissue depth
>50% of repair tissue depth or total degeneration
4. Structure of the repair tissue
Homogenous
Inhomogenous or cleft formation
ondral bone plate and marrow. The signal intensity
repair tissue was separately determined in fast spin-
(dual T2-FSE) and fat-suppressed gradient-echo (3D-
S) sequences and a complete repair was graded as
ense if it appeared as intense as the adjacent native
ge.
cording to the first published classification system,
marginal modifications were performed to obtain repro-
e results and clear definitions. Thus, the variable syn-
was modified to the variable effusion. The appearance
usion is defined when the accumulation of fluid in the
ial joint increases more than 1 cm in any section of the
Clinical outcome
r the description of the clinical outcome of the patients,
sed a standardized evaluation system, which was
ned for the description of cartilage repair procedures
ationwide registry (CARRERA: Cartilage Repair Reg-
Austria). This system includes subjective and objective
me scores and provides a computerized analysis tool.
e analysis used in this study, subjective patient evalua-
f validated scores were used, specifically, visual analog
(VAS) and knee injury and osteoarthritis outcome score
S) [15–17]. KOOS is a 42-item self-administered, self-
natory questionnaire that covers five patient-relevant
>50% of repair tissue depth or total degeneration
4. Structure of the repair tissue
Homogenous
Inhomogenous or cleft formation
5. Signal intensity of the repair tissue
Dual T2-FSE
Isointense
Moderately hyperintense
Markedly hyperintense
3D-GE-FS
Isointense
Moderately hypointense
Markedly hypointense
6. Subchondral lamina
Intact
Not intact
7. Subchondral bone
Intact
Non-intact (edema, granulation tissue, cysts, sclerosis)
8. Ahesions
No
Yes
9. Effusion
No
Yes
s r e p r e s e n t a t i v e o f t h e a v e r a g e q u a l i t y o f c a r t i l a g e r e p a i r . a , b T h e T 1 c o r o n a l
p o s t - o p e r a t i v e l y ) o f t h e l e f t k n e e s h o w c o m p l e t e d e f e c t f i l l i n g o f t h e m e d i a l](https://image.slidesharecdn.com/maciversusonestagesiot16-180118162713/85/Tecnica-MACI-versus-le-tecniche-one-step-17-320.jpg)