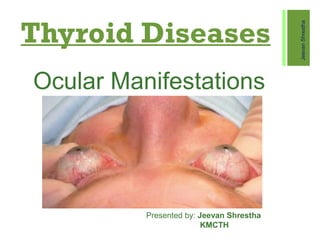
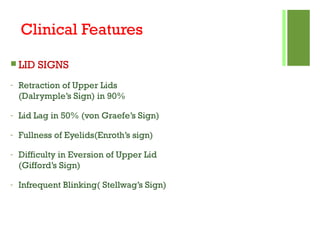
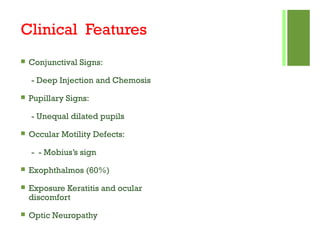
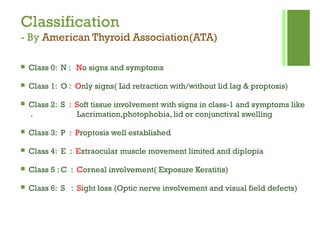
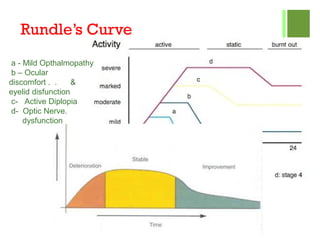
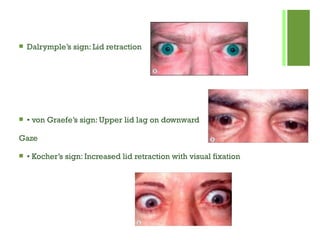
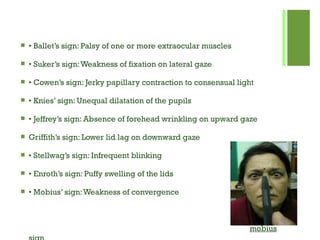
This document discusses thyroid diseases and their ocular manifestations. It focuses on Graves' disease, which causes Graves' ophthalmopathy - an autoimmune inflammatory disorder affecting the eye area. Symptoms include eyelid retraction, swelling, redness, and bulging eyes. Risk factors include female sex, smoking, and preexisting thyroid conditions. The document outlines pathogenesis, clinical features classified by severity, diagnostic tests, and treatment options including medications, surgery, and radiation therapy.