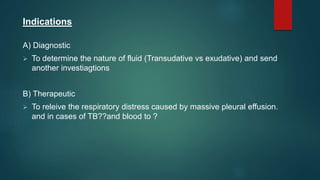
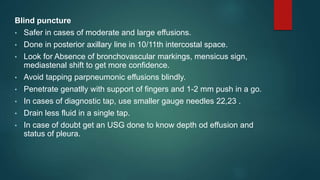
1. Thoracentesis is a procedure to drain fluid from the pleural space for diagnostic or therapeutic purposes. It can be done blindly or under ultrasound guidance.
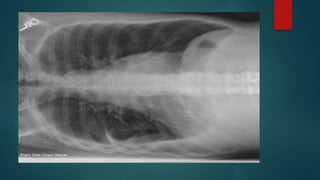
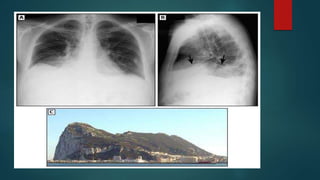
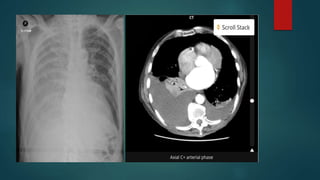
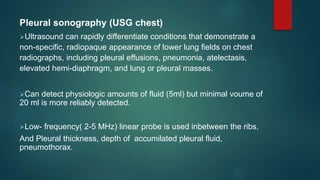
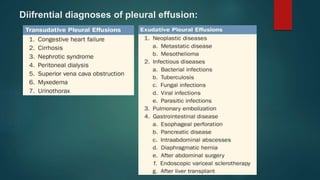
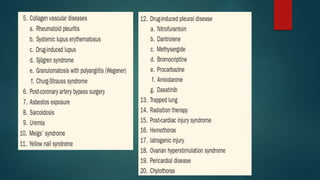
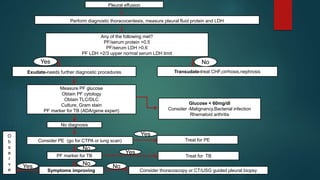
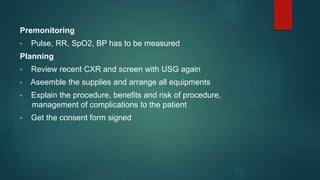
2. A thorough history, physical exam, chest x-ray and ultrasound are used to evaluate pleural effusions and determine if thoracentesis is needed. Samples of pleural fluid are analyzed to identify the cause of the effusion.
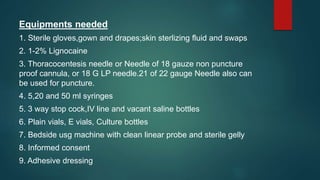
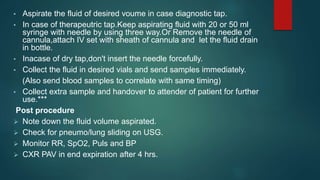
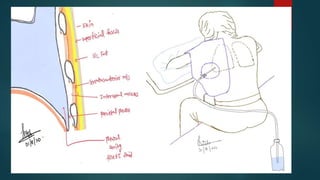
3. Thoracentesis involves inserting a small needle between the ribs to drain pleural fluid. Samples are taken for analysis and the procedure provides relief for patients with large effusions. Complications can include pneumothorax, infection and bleeding.