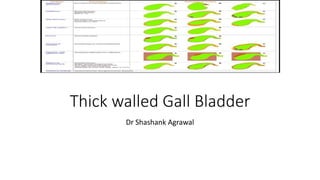
Gallbladder wall thickening can indicate various conditions, and distinguishing between benign and malignant causes is crucial for appropriate management. Risk factors for gallbladder neoplasms include gallstones and chronic cholecystitis, with imaging techniques playing a significant role in diagnosis and differentiation. Proper surgical approaches are essential, particularly to avoid compromising treatment for malignancies.